If someone has Panic Disorder, they experience “panic attacks”, which seem to come on all of a sudden, for no apparent reason. In Panic Disorder, panic attacks can occur in a variety of situations e.g. at a friend’s house, walking down the street, looking after your grandchildren or whilst you are at home.
People have recurring and regular panic attacks. Over time, people are anxious anticipating having another panic attack and are fearful of the consequences of having panic attacks. To avoid having another panic attack, or to avoid feeling embarrassed in case they have a panic attack in front of others, people can withdraw from going out/doing things/seeing people. Panic attacks can occur in other anxiety conditions and can occur infrequently without meeting criteria for Panic Disorder.
Panic attacks are an intense feeling of anxiety characterised by experiencing at least four of these symptoms:
- Trembling or shaking
- Sweating
- Hot flushes or cold chills
- Numbness or tingling sensation
- Breathing difficulties
- Chest pain
- Palpitations – “racing” heart
- Feeling of choking
- Dry mouth
- Feeling sick or stomach pain
- Feeling weak, faint, or dizzy
- Feeling like you are losing control
- Feeling that things are distant or that you “are not really there”
- Fear that you are going to die.
Panic attacks start suddenly. The intense feeling peaks quickly but can typically last between one and ten minutes, however, people can feel anxious, fearful or drained for a longer period of time following this. These panic attacks can be described as a ‘false alarm’, where someone thinks that they are threatened when there is not a real physical threat.
People of all ages can experience panic attacks. Around one in 10 people can experience occasional panic attacks, which are often triggered by stressful events such as, difficulties in relationships, work demands or experiencing loss. It is also quite common for people with Panic Disorder to experience other mental health difficulties, for example, Depression or Agoraphobia (avoiding places; please see other pages for these conditions). If panic attacks are experienced consistently with only certain objects or situations, it may suggest a Phobia rather than Panic Disorder (see Phobias page). Panic Disorder can occur for a number of reasons which include; someone’s biological makeup, personality, ways that people have learned to deal with distress and in the context of stressful events.
More Information
What helps
Many people can experience a panic attack. However, if you experience repeated panic attacks and you are fearful about having other panic attacks, you most likely have Panic Disorder. It would be helpful for you to speak to your GP in the first instance. It is important to check with your GP that any of the physical symptoms associated with panic attacks are not due to a physical condition.
There are a number of treatments that are effective in treating Panic Disorder:
Self Help Materials
If you have mild difficulties, reading information about Panic Disorder may be enough to help you. Please see the ‘find out more section’ for self help materials.
Psychological Therapy (‘talking therapy’)
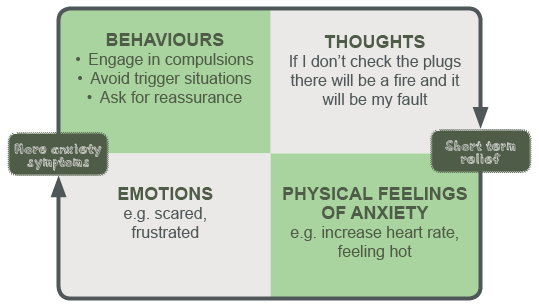
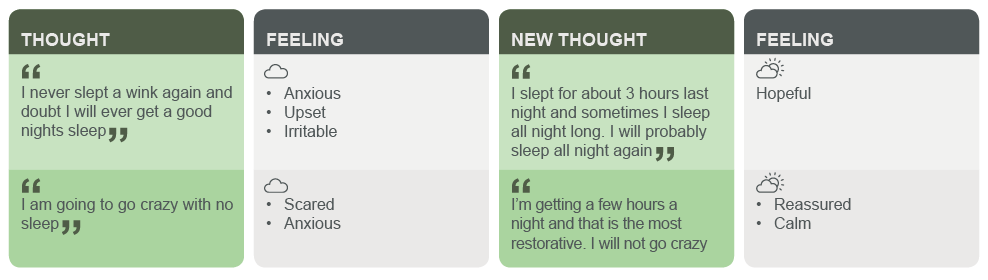
If your difficulties with Panic Disorder are having more of an impact on your day to day life, your GP might refer you to a Primary Care Mental Health Team or a Community Mental Health Team. You can also refer yourself to a Primary Care Mental Health Team in your area by searching for one on the internet. These teams have a range of staff (for example, Mental Health Practitioners, Cognitive Behavioural Therapists and Clinical Psychologists), who are trained to help people with these difficulties. If you are having more severe difficulties with Panic Disorder, it would be best for you to work with a professional to engage in a structured “talking therapy”. Cognitive Behavioural Therapy is a talking therapy that helps you to see the relationship between your thoughts, feelings, physical sensations and behaviours. By exploring and questioning your thoughts and changing some things that you do, this can help you to feel better. There is evidence to suggest that group work, internet-based interventions and one to one work with a therapist are effective in treating Panic Disorder. Again, based on how severe your difficulties are, this could involve engaging in 4 to 20 sessions. Each session usually lasts one hour.
Medication
Anti-depressant medication is often used to treat depression, however, there is evidence to suggest that anti-depressant medication is also effective in treating anxiety disorders including Panic Disorder. The National Institute for Health and Care Excellence (NICE) produced guidelines suggesting that selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) are the most effective anti-depressants in treating Panic Disorder. There can be a number of side effects of using anti-depressant medication, therefore it would be best to discuss this with your doctor.
Living with…Panic Disorder
If you have Panic Disorder it is expected that you will worry about having another panic attack. You might also worry about what the consequences of having a panic attack will be, for example, “will I lose control?” or “will I die?” You might find that as you are worrying about having another attack, you might not able to focus on work or conversations with others as well. You may want to avoid going out (see Agoraphobia in Phobia section) or doing certain things. You might notice that your overall anxiety/stress levels are higher. If you are older you might think that you should not be having these difficulties at your age. We know that having difficulties with your mental health is just as common at any age.
Looking after someone with…Panic Disorder
If someone has Panic Disorder they will be scared of having another panic attack. They might not want to discuss their difficulties with you or they may stop going out or wanting visitors. Breathing plays an important role in keeping panic attacks going. When people are anxious, their breathing changes which can cause other physical changes in their bodies for example, feeling light headed or an increase in their heart rate. If someone has a panic attack when they are with you, encourage the person to take regular, slow breaths for at least a few minutes. You could try giving them reassurance such as ‘I’m with you’ or ‘this feeling will pass’.
It would be helpful for the person experiencing Panic Disorder if you could encourage them to attend their GP, or if you were able to, you could offer to go with them. It would be important for the person to know that there is a range of treatments that can help with how they are feeling and that they are effective. You might want to give them some information on Panic Disorder which is in the ‘Find out more’ section.
Also, remember to look after yourself. It can be stressful supporting someone who is experiencing these difficulties.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Further information and support
This is a short handout on panic attacks and Panic Disorder from the Centre for Clinical Interventions.
The Glasgow Wellbeing booklet titled Panic Attacks includes information about panic attacks and self-help interventions:
The Centre of Clinical Interventions has a range of work modules, including Panic Stations, that you can work through yourself.
These are some self help work sheets that provide information about Panic Disorder and some techniques that you can use to help:
Useful contact:
No Panic – a voluntary charity which provides information, gives peoples accounts of living with Panic Disorder (and other anxiety difficulties) and has materials which you can purchase.
There is also information for people that are trying to support someone with these difficulties.
There is also a helpline so you could speak to someone – 0844 967 4848 – (Everyday 10.00am – 10.00pm, charge: 5p a minute + your access charge)
BSL – Panic Disorder
NHSGG&C BSL A-Z: Mental Health – Panic Attack
Panic attacks are sudden periods of intense anxiety which appear to have no obvious triggers or reasoning. They can happen when a person least expects it and can be very distressing and frightening for the person. They can be accompanied by physical symptoms such as a racing heart, feeling faint or dizzy, sweating, trembling, feeling shaky, breathlessness and agitation. The person may feel like they are losing control or dying.
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde