Stress is the experience of the feeling that the demands upon us are greater than our resources to cope. People can cope with many difficult tasks but when an extra task is added they feel stressed, one extra demand on someone’s resources can push them into feeling stressed, as described by the phrase ‘it was the straw that broke the camel’s back’.
Stress can be an overwhelming experience and can be understood as pressure from others or being put in situations that you find difficult to cope with. It can also occur when you feel that you don’t have much control over a situation.
More Information
Where does stress come from? The Flight or Fight Response…
The ‘Flight or Fight’ response
The ‘fight or flight response’ is our body’s own protective response to danger and, in essence, it is a mechanism designed to protect us, and not as it feels, destroy us.
Our bodies are designed to respond to danger; we have an inbuilt defence mechanism known as the ‘fight or flight response’, which triggers psychological and physical changes in our bodies. The release of chemicals can give very real physical symptoms such as rapid heart rate and breathing. These symptoms are designed to give us the ability to ‘fight or flee’ a specific danger, however for a panic attack sufferer, someone who suffers from anxiety or someone experiencing stress, these feelings can feel intensified and with no present danger.
Why do we have the “Flight or Fight” response?
This sudden burst of adrenaline, the increased oxygen and heart rate, gives our bodies increased abilities and sensory perception – which if you need to flee a wild beast or save your family from a burning building will indeed be used to maximum effect. If however you are simply doing your grocery shopping, taking your child to school, or sat watching TV for example, these frightening feelings can be extremely difficult to cope with or explain.
If there is no need to use the excess chemicals; adrenaline or the increased oxygen supply, then our bodies begin to act against us, the decreased carbon dioxide levels in our lungs and blood causes us to feel dizzy and disoriented, we can begin to hyperventilate and a panic attack can ensue.
What can I do to help if I feel stressed?
There are a range of things you can do if you feel like you are stressed regularly. There are physical activities and mental tricks you can try to help; some are activities you can implement when you are in a stressful moment and others are things you can do to try and reduce your overall stress levels and prepare for future challenging times.
- Be Active
- Take Control
- Connect with people
- Have some me time
- Challenge yourself
- Avoid unhealthy habits
- Work smarter not harder
- Be positive.
Living with stress – how does stress feel?
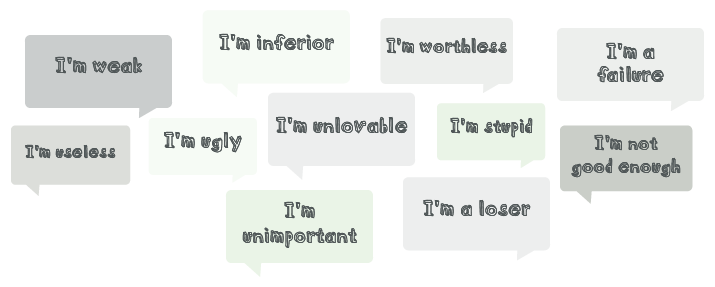
Stress is frequently described as the feeling of being under pressure. Some people describe feeling under threat, anxious, tense, tearful or agitated. Often these feelings are accompanied by physical sensations. It is important to note that these reactions are normal but everyone experiences stress in their own way so your reaction may appear to be different from a friend or family member’s.
If stressful times pass, the body will usually return to normal functioning after a period of time. However if you feel that you have been stressed for some time you make be advised to seek support from your GP.
Looking after someone with…stress – how might we notice if someone is stressed?
When people are stressed they can make choices they would not usually make and behave in a way that is a little different from usual. From the outside you might notice a person saying or doing things that are out of character, someone struggling to concentrate, physically appearing more tired than usual, eating and drinking more or less than usual, taking more or less time over their general presentation than usual and/or appearing to be rushing or forgetful.
Stress is something many people feel for short periods in life but difficulties arise if this experience persists.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
How can I support someone else who seems stressed?
Whilst the above resources will be helpful for your understanding of stress, the award-winning Power of OK campaign from Scotland’s See Me programme gives some very practical advice and contains an accessible video resource to explain all (videos contains strong language)
Further information and support
One resource you may find helpful for coping with stress is the Glasgow Wellbeing resource, which includes a free guide to download, and relaxation videos. In addition, the website has a range of other support materials to help you think about the causes of stress.
Glasgow Wellbeing is full of helpful and informative resources
NHS Choices suggest 10 tips to beat your stress.
This is an NHS resource with instructions for breathing exercises, which are recommended to help ease the feeling of stress
Resources created specifically for young people
The Royston Stress Centre which offers an outreach service to 11–18 year olds in North Glasgow have made an excellent film to help young people understand stress:
Ayemind website contains child-friendly resources explaining stress and includes information on child-specific stressors such as school exam stress
The Royal College of Psychiatrists have a leaflet for young people who are managing stress
A free mobile application called SAM – Self Help for Anxiety Management – has some useful resources and can be carried around with you subtly on your phone
SafeSpot is a brand new app for iPhone and Android that promotes positive mental wellbeing in children and young adults.
If you need someone to talk to
Breathing Space Scotland has a phone line and an associated therapy service called Living Life
Samaritans offer a 24/7 confidential support service which includes a phone line: 0141 248 4488, a freephone number: 116 123 and an email service: jo@samaritans.org
BSL – Stress
NHSGG&C BSL A-Z: Mental Health – Stress
Stress is normal and it affects everyone. It usually happens when you are in a situation that puts you under pressure. It can happen when you have lots to think about or do or when you don’t feel you have much control over a situation. It usually happens when you have things to do that you find difficult to cope with. Many situations can cause stress including relationships, work demands, financial worries and so on. It can have an effect on our emotions, thoughts, behaviour and physical wellbeing
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde