Referral Process – How to refer a patient
Referrals to the national complex mesh surgical service will be accepted from any Urogynaecology service in Scotland.
- The local urogynaecology consultant will have reviewed the patient clinically and agreed with the patient to refer to the service in Glasgow for consideration of partial or total mesh removal.
- The consultant will refer the patient using the agreed Multidisciplinary Team (MDT) referral form.
- The GGC MDT will discuss the patient, review all the information provided by the local urogynecologist and recommend a treatment plan.
- The patient will then be contacted by both the psychology service and the clinical nurse specialist for support and information regarding what to expect at their forth coming clinic appointment.
- The patient will attend the clinic and meet the team.
- They will discuss the proposed treatment plan and any surgical options available to them.
Mesh appointment
We recognise that Every Woman is Different and will have different needs and thus every stage of patient treatment is determined by a team of experts working closely together to provide individualised care.
Patients referred to the service will be seen through the specialised mesh clinic by a team of clinicians along with other members of the MDT. We will obtain as much information about your mesh implant and any treatment carried out to date from your local unit. Patients will have full assessment (history and examination) and will be offered investigations as appropriate.
Investigations can include:
- Cystourethroscopy (telescopic assessment for bladder and urethra)
- Ultrasound scan – Translabial /transperineal and endovaginal
- MRI scan
- Other investigations like sigmoidoscopy (telescopic exam of lower bowel), Examination under anaesthesia , diagnostic laparoscopy and CT scan can be requested if deemed necessary.
We may ask some of the above tests to be done at your local hospital for your comfort and convenience.
Your case will be discussed at our complex mesh MDT and the outcome will be relayed to you by one of the surgical team members and further appointment/s will be arranged.
Surgical Treatment options offered :
- Injection of local anaesthetic and steroids
- Conservative surgical/minimum access procedures using Laser
- Partial mesh removal (removal of exposed vaginal mesh) and (part or whole of vaginal portion of the mesh)
- Complete mesh removal
- Removal of vaginal and extra vaginal portion/s of mesh
- Groin dissection
- Partial and complete removal of abdominal inserted mesh for prolapse.
Team offers both open and laparoscopic (key hole) approach.
Information about above surgical procedure can be accessed by clicking here and about the perioperative process here.
Clinical Nurse Specialist
Complex Mesh Specialist Nursing
Nurses within the Complex Mesh Surgical Service are Specialist Urogyneacolgy trained who have an expert knowledge and understanding of the use of mesh for the treatment of Pelvic Organ Prolapse and Stress Urinary Incontinence. We understand the potential physical and emotional impact of the complications experienced from the use of mesh. We aim to offer person-centred care throughout your journey through the Service.
Our role within the Complex Mesh Surgical Service is to provide care and support to all individuals within the clinic setting.
We recognise that it can sometimes feel overwhelming to attend hospital appointments. We are there to offer support throughout, to ensure you feel able to voice any concerns you may have, to discuss any difficulties you may experience and to help you to identify your goals for treatment.
We will contact you prior to your first multidisciplinary clinic appointment to introduce ourselves and answer any questions about the clinic that you may have. We will then be there to support you during your multidisciplinary clinic appointment, and throughout your journey with the service.
If you undergo mesh removal surgery, we will meet with you with in the ward before you are discharged home from the Hospital. We will arrange a dedicated time for post-operative telephone follow-ups.
In addition, it is important to us that people using the service are aware that we can be contacted at any other time by telephone, should there be any queries or concerns (see ‘Contact Us’). We aim to support you to achieve the best possible outcomes for you as an individual.
Lifestyle advice
The Complex Mesh Surgical Service
Lifestyle Information
This information is to help you know what you might be able to do in the days or weeks before any mesh related surgery. This will speed up your recovery and help you get the best outcome possible.
Even small positive changes in lifestyle make a difference and encourage you to be as healthy and strong as you can be.
Lifestyle changes that target your activity, weight and diet may help your bladder and bowel symptoms.
Being Active
Being active is one of the best things we can do for our physical and mental health.
Sometimes it can be hard to stay active when we have pain, leakage from the bladder or bowel, or struggle to find the motivation. Even small amounts of regular activity can make a difference.
The following tips might help:
- Start with small and regular activity that you enjoy and that is easy to do such as walking, or suitable exercise classes
- Try and find an exercise partner to help you stay motivated
- Plan to be active every day
- If you already go to classes, ask the instructor to help you with easier options for when you feel less strong or more uncomfortable
- Work towards increasing your daily activity over time
We know that physical activity can boost self-esteem, mood, sleep quality and energy.
The Government guidelines are shown below BUT not everything will suit everyone – get advice on the right strength training for you.

Managing your weight
A healthy weight is important for overall wellbeing and can help you prevent and control many diseases and conditions. National guidelines recommend that a body mass index (BMI) of less than 30 can help reduce symptoms of mixed urinary incontinence and prolapse. The link below will give you general information about the effects of a high BMI on your pelvic floor and the risk of complications during and after surgery.
Losing weight can be hard and you may need lots of help and support:
- Ask your friends to help you
- Speak to your GP
- Find out what is available locally
The links below may be useful:
- 12 Week Weight Management Programme
- How to lose weight safely – Food and nutrition
- Lose weight – Better Health – NHS
- Managing your weight – NHS
Have a healthy balanced diet
What you eat and drink is very important for bladder and bowel health. Staying active also helps.
Fluids
It is important to drink enough each day even if you have bothersome bladder symptoms. Try to drink at least 1.5litres to 2litres of fluid per day. You may need to increase your fluids gradually to help retrain your bladder. It is recommended that you limit the amount of caffeine and fizzy drinks such as coke, coffee, energy drinks and alcohol because they are known to irritate the bladder.
Drinking enough may also help with constipation and encourage a regular bowel habit.
Food
A balanced diet with enough fibre and physical activity can help to regulate your bowel movements, prevent constipation and improve rectal emptying. The right stool consistency may help manage symptoms of bowel urgency and leakage of poo.
Understanding how to have the right stool consistency is particularly important at the time of surgery to help prevent straining and constipation post operatively.
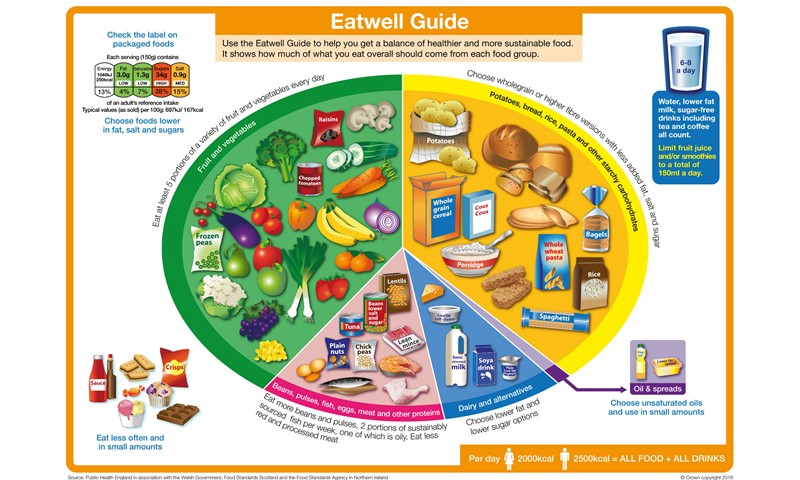
The Eatwell guide from the NHS gives an idea of what the balance of foods should be.
Further information and help is also available from the following links:
Other lifestyle modifications which may help manage pelvic floor symptoms
- Stopping smoking and managing any respiratory conditions such as asthma may reduce your cough. You may also feel fitter and more able to take part in physical activity. This in turn can benefit your mental health and wellbeing.
- Reducing alcohol intake. Alcohol is known to irritate the bladder. Other benefits of cutting down may be improved mood, sleep quality and feeling more energetic
For further help with this, see you GP for local services and have a look at the following website pages:
If your ability to make helpful lifestyle changes are not possible due to low mood, please seek help to find the right support for you.
Got a date for surgery?
Knowing what to expect from surgery can help reduce preoperative anxiety. The following link and short video will help to support and guide you:
You will also be seen ahead of your operation to get information on pre and post operative care.
Psychology
Complex Mesh Clinical Psychology Service
Clinical Psychologists are trained to have an expert understanding of how people think, feel and behave. These skills are used to help people cope with difficult situations, feelings, and experiences.
We recognise that complications from mesh for pelvic organ prolapse or incontinence have the potential to result in exceptional challenges that people may not ordinarily face. We also understand that it can be difficult to cope with these difficulties alone.
Our role within the Complex Mesh Surgical Service is to provide support to individuals for any mesh-related difficulties they may encounter. We recognise that in addition to the expert care of your physical needs, having good social and psychological support is an important part of your overall wellbeing.
Our aim is to meet with as many people in the Complex Mesh Surgical Service as we can. This allows us to introduce ourselves, as well as assessing whether you have any concerns relating to mesh that we could address together.
We do this by:
- Offering an initial appointment with a Clinical Psychologist prior to assessment by the multidisciplinary team (MDT)
- Attending MDT clinic appointments
We also offer appointments to anyone who requests support at any stage in their assessment or treatment within the Complex Mesh Surgical Service. If there are mesh-related difficulties that you would like help with, we offer individualised support.
This may include:
- One-off discussions or suggestions
- Individual appointments (by telephone, video call or face to face)
- Joint working with other professionals (e.g surgeons, physiotherapists, GPs)
- Signposting to other services
If you would like our support, you can let us know by speaking to us (in our appointment prior to the MDT clinic appointment, or in the MDT clinic appointment) or by telling another member of the Complex Mesh Surgical Service. Please note that we are only able to accept referrals for people who are being seen within the Complex Mesh Surgical Service.
Information on what to expect from sessions with a Clinical Psychologist within the Complex Mesh Clinical Psychology Service, can be found in our patient leaflet.
Contact us
To request or ask about support from the Complex Mesh Clinical Psychology Service, please speak with any member of the Complex Mesh Surgical Service MDT.
If you are struggling with low mood and cannot wait to speak to someone, please contact your GP for advice, or call NHS 24 on 111.
The following organisations can also offer an immediate ‘listening ear’:
Samaritans 116 123 (free 24-hour helpline)
Breathing Space 0800 83 85 87 (free helpline, 6.00pm to 2.00am weekdays, 24 hours at weekends)
Physiotherapy
The Complex Mesh Surgical Service
Physiotherapy is now considered as one of the first non-surgical options that should be offered for the management of stress urinary incontinence and for prolapse.
Pelvic Health physiotherapists have undergone additional training and have specialist expertise in bladder, bowel and vaginal health. Our goal is to support and work with people to lessen the impact of pelvic floor problems and help restore their quality of life. Common pelvic health problems may be bladder and bowel incontinence or emptying difficulties, prolapse and painful sexual intercourse. Physiotherapy aims to improve function and minimise the symptoms that can impact on the physical and psychological aspects of life. Education and understanding of the anatomy and function of the bladder, bowel and pelvic floor muscles is a key part of this.
Why is there a specialist physiotherapist in the Complex Mesh Surgical Service?
- Many of the women seen in the Complex Mesh Surgical Service (CMSS) may have seen a physiotherapist already and the specialist physiotherapist can help to decide whether further physiotherapy input will be of benefit.
- People attending the CMSS may come from all over Scotland. The specialist physiotherapist will share information, advice and expertise with the physiotherapists who may be involved in the agreed management plan. We aim to ensure continuity of care within the local setting.
Who can be seen in the Complex Mesh Physiotherapy Service?
Physiotherapy is a key component in managing mesh related pelvic floor problems and if indicated the specialist physiotherapist will aim to see all the people attending the CMSS. If the physiotherapist is not available on the day, and further physiotherapy is needed, a referral will be made.
How can a specialist physiotherapist help?
The physiotherapist in the CMSS will give you an opportunity to talk about your current symptoms and help you to understand what might make a difference and improve your quality of life. This may include:
- Discussing bladder, bowel, vaginal or rectal symptoms such as incontinence, urgency, frequency, sexual discomfort and pain
- Reviewing lifestyle habits that may be contributing to current symptoms
- Signposting to other sources of information that may help with encouraging good bladder and bowel habits
- With consent, the specialist physiotherapist may do a vaginal or rectal examination to assess the pelvic floor muscle strength, tone, relaxation and pain.
- Feedback will be given on examination findings and a treatment plan will be discussed and agreed.
- Providing sources of further information including links to reliable patient information sites
Where surgery is the agreed plan, physiotherapy support will be provided before and after your surgery (link to the pre op and post op info tbc)
Useful Links and Resources
Pain Services
Consultant Anaesthetists at complex mesh surgical service have experience in looking after patients referred to the Centre/Service with complications related to mesh used for stress urinary incontinence and pelvic organ prolapse. They work as part of multidisciplinary team and will be present at the complex mesh clinic.
The role of the Consultant Anaesthetist is to carry out risk assessment, pain assessment and assess suitability for surgery. Some conditions will require further investigations and/or optimisation prior to surgery to minimise those risks, which is usually done via referrals to the patient’s GP or other health practitioners.
If opting for surgery Consultant Anaesthetist will discuss what post-operative pain management techniques are available and risks associated with each.