IPCAT (IPC Audit Tool) User Guides:
- SICPs Tool – Acute/MH
- QA Tool – Acute
- QA Tool – MHP
- Updated SICPs Clinical Area Summary Document (Oct 22)
IPCAT (IPC Audit Tool) User Guides:
Healthcare Improvement Scotland (HIS) Healthcare Associated Infection (HAI) Standards
The prevention and control of infection throughout healthcare is everyone’s responsibility and is a major component in the drive towards a safer NHS Scotland.
These Standards are one part of the drive for a safer NHS Scotland, so should be seen as complementary to HAI and patient safety work undertaken by other bodies, e.g. Scottish Patient Safety Programme (SPSP). These Standards for HAI apply to all healthcare environments in which patients are treated.
New South Glasgow Hospitals is the largest capital healthcare project in the UK and forms the keystone within NHS Greater Glasgow and Clyde’s (NHSGGC) Modernisation Strategy. The hospitals provide new state of the art healthcare facilities and high quality designed environments for a significant proportion of the population of Glasgow, and in some fields, for Scotland. Opened at the end of April 2015, the Queen Elizabeth University Hospital is Scotland’s largest ever publicly-funded NHS construction project, costing £842 million to build. The project brings together Children’s and Adult Acute services with existing Maternity, Neo-natal and Neurosciences services on one campus. It has the biggest critical care complex and one of the biggest Emergency Departments in Scotland providing a brand new 14-floor adult hospital with 1,109 beds. The new children’s hospital, with a separate identity and entrance, adjoins the adult hospital, with 256 beds over five storeys.
Each building has a distinctive character, with artwork and colour schemes specially selected to enhance wellbeing and to give useful landmarks which can act as signposts.
Ginkgo Projects working with Gillespies (masterplanners and landscape designers) and Nightingales (architects and interior designers), were contracted by Brookfield Multiplex to develop and deliver the Therapeutic Design and Arts strategy and programme for the New South Glasgow Hospitals. The Design and Healthy Environment Strategy Group at NHSGGC has overseen the development of this programme.
Ginkgo’s evidence-based programme for the Therapeutic Design and Arts strategy has sought to enhance the patient experience and journey through developing creative processes and works of art and design that aim to connect patients, staff and visitors to the hospital’s social cultural and environmental context. Working closely within the project design team, Ginkgo Projects has developed a programme which promotes patient dignity and distraction through exploring social, cultural and environmental connections. The strategy was produced in collaboration with two artists Donald Urquhart and Will Levi Marshall. Seven core projects were commissioned resulting in over 600 individual works of art. The approach has been to integrate work that provides as much impact as possible within key navigation points, waiting and treatment areas.
Ginkgo provided a direct service for the curation, design and implementation of all projects working closely with its teams of artists and designers in close collaboration with the NHSGGC and Brookfield Multiplex project teams.
Art and Therapeutic design programme for the New South Glasgow Hospitals (2010-2015)
The programme is composed of seven lead projects as below:
Matthew Dalziel and Louise Scullion led a team of artists to create artworks for eight floors of the acute adult hospital (The Beacon). These occupy three types of spaces: Lift Spaces, Corridor Spaces and in the Socialisation Space / Room at the end of each corridor. Work has been coordinated in layers of artworks that look at eight broad Scottish habitats drawing the wider landscape of Scotland into the building.
Over 250 works have been produced. The project has used existing images produced by Dalziel and Scullion made over a lifetime of exploring Scotland’s diverse landscape – together with many new works made specifically for the project. Other artists include: Nickolai Globe (ceramic works for Socialisation Spaces), Patricia & Angus Macdonald (areal views of Scotland, establishing the examined habitat themes), Ursula Bevan (creation of a ‘family’ of characters that explore each of the themes – the final works being rendered as styalised lino cuts), Beka Globe (striking black & white images exploring a selection of the themes, with a particular focus on the western isles), and Frances Walker (a smaller group of works that capture Frances’ unique distillation of geology in her complex drawings of landscape).![]()
Dalziel and Scullion, Lift core numbers. Photograph Ruth Clark![]()
Nickolai Globe, Ceramic cases in preparation. Photograph Dalziel and Scullion![]()
Nickolai Globe, Ceramic cases in socialisation spaces. Photograph Ruth Clark![]()
Beka Globe, Research work for Beacon project. Photograph Dalziel and Scullion
Graphical House, Haa Design and artist Rachel Mimiec designed twenty one land marks for key areas and thresholds of the podium building of the new hospital.
Rachel undertook research and workshops within the Govan community and at a number of the hospitals working with patients and staff to find out what was memorable in their journey from home to their work place.
As Rachel gathered staff stories, Graphical House designed the panels using simple striking imagery. Poet Robin Wilson condensed the stories into short texts embedded within each landmark. Singular unexpected objects from each story form the basis of each design providing memorable interventions at key decisions points.
The landmarks all have a similar style and identity composed of white Corian with the designs inset in coloured Corian. The panels wrap around a corner and are built out with a deep coloured edge to match the design.
One external landmark is composed of a grid of bold squares relating to the colours that have been used internally and references a patchwork quilt. Graphic images from the internal landmarks are woven into the external piece so that there is a connection between inside and outside.
Interior Specialist Surfaces, Landmarks in fabrication. Photograph Beccy Lane
Four artists worked with children and young people at the Royal Hospital for Sick Children at Yorkhill during a programme of artist residencies in 2013 led by Alison Unsworth. Emma Varley worked with the Department for Child & Family Psychiatry; Frances Priest worked with children at Yorkhill; Ian Richards worked with young people at Yorkhill; and Alison Unsworth worked with children and young people at Yorkhill and local schools.
Time was spent talking, drawing, cutting, sticking, writing, scrunching, colouring, thinking, looking, and sharing ideas for artwork which might go on the walls of the new children’s hospital. Following the residencies, a series of artworks were designed to be installed on the walls of the new children’s hospital across 90 locations.
Frances Priest worked with shapes, motifs and patterns, inviting children to play with them, arrange them and imagine what they might be. She has used the drawings made by children during the residency to create a series of artworks based on four themes; circus characters, climbing characters, birds and space travel.
Ian Richards used letra set transfers, asking young people to write a sentence or phrase, building narratives by passing on one person’s writing to somebody else and asking them to respond to it. He worked with young people to digitally create a series of bold, colourful patterns based on the repetition of one motif. Ian has developed the phrases, stories and patterns created during the residency into a series of artworks combining patterned Scottish mountain ranges, tower blocks made out of bread, hot air balloons and a cast of funny bird characters!
Alison Unsworth created the Unfinished Places newspaper in collaboration with children and young people at three local schools close to the site of the new hospital. Unfinished Places is a newspaper for children and young people. It’s full of pictures which are only half finished and we asked for help to complete them by drawing, writing or sticking things in. Pages from the returned newspapers can be seen at yorkhilldrawings.com. Alison’s artwork for the new hospital is based on four themes relating to life in Glasgow and the wider Scottish landscape; wildlife, habitats, transport and buildings or structures. She selected imagery relating to these four themes and combined it together to create different scenes, influenced by a selection of ideas, drawings and stories from the returned newspapers and from artwork created by children and young people at Yorkhill.
Emma Varley worked closely with staff in the Department for Child and Family Psychiatry, considering how the images she created might be used in part to assist therapy or influence behaviour. She has created a series of artworks combining detailed line drawing with coloured shapes and graphic motifs. The artworks include familiar, domestic objects such as a toothbrush and toothpaste or a pair of shoes, alongside household furniture and friendly animals such as a cat and a fox. All of the imagery was carefully chosen in collaboration with staff in the department.
A library of over 100 designs has been created for future application as required.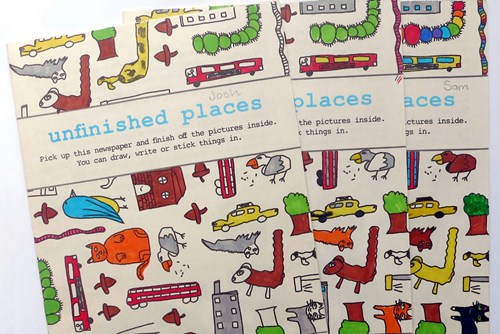
Unfinished Places newspaper produced as part of the artist residencies. Photograph Alison Unsworth
Ian Richards, Graphics integrated into new childrens’ hospital. Photograph Ruth Clark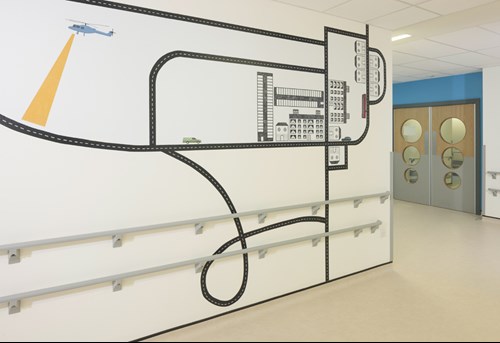
Alison Unsworth, Graphics integrated into new childrens’ hospital. Photograph Ruth Clark
Alison Unsworth, Graphics integrated into new childrens’ hospital. Photograph Ruth Clark
Emma Varley, Graphics integrated into new childrens’ hospital. Photograph Ruth Clark
The Dignified Spaces team was led by Alex Hamilton and included Fremi Arts – art commissioning and curatorship, Catalog Design – interior design, Jane McKie – creative writing, Anna Channing – medical herbalist, Marco Scerri – visual communication, Hannah Brackston – green spaces research. Nicola Murray developed the wallpaper and textile design which was then delivered by Teal Furniture Ltd.
Up to eighty quiet rooms were considered and enhanced as part of the core project. The rooms are used for a range of purposes of which the most important are conversations between clinical, nursing or spiritual care staff and patients’ relatives and carers. On a practical level the rooms need to be comfortable, safe and quiet; they also need to convey that users of the rooms are being treated with dignity.
The team worked with an art and design palette, including lighting, wall colours and coverings, flooring, furniture and artworks. The project used creative community engagement strategies to inform thinking about the idea of dignity and the development of innovative approaches to interiors.
The approach was to seek connections with nature, this approach can be called biophilic design.
Hamilton and his team settled on the metaphor of walled garden to inform the design process.
To drive the biophilic design, a process of creative engagement was undertaken. The community workshops and clinical conversations involved individuals aged from four to seventy, exploring ways of considering all aspects of dignity, including how to listen, and what helps listening in clinical settings.
The workshop activity, held at Hidden Gardens, Glasgow, involved participants looking at the plants within the walled garden, selecting leaves and petals with which they made their own image using the cyanotype process. Cyanotype photography provided a direct and immediate method for image making. These pictures helped to inform the design process, wallpaper, fabric for chairs, and the overall aesthetic used in the Quiet Rooms.
Through close collaboration with Teal a unique fabric design was developed and applied to standard furniture for each of the rooms. This fabric range is now an available product within the Teal range.
Alex Hamilton, Cyanotype workshop at the Hidden Gardens. Photograph Alex Hamilton
Alex Hamilton, Cyanotype print produced from workshops. Photograph Alex Hamilton
Alex Hamilton, Dignified Spaces quiet room. Photograph Ruth Clark
www.alexanderhamilton.co.uk
The 100 Flowers project is a response to the restriction of real flowers in acute hospitals, due to infection control measures, and is designed to put flowers back at the heart of the experience of the new hospitals.
The iconic image in the collection is a photograph taken by a member of staff. It’s of a small group of daffodils in the grounds of the Southern General. Craig Humanuth, the member of NHSGGC staff who took the photograph, commented that these are the only flowers he sees during his working day. In the background you can just make out the new Hospitals reflected in the windows of the old one.
The 100 Flowers project has produced a hundred new works of art of flowers in the New South Glasgow Hospitals in waiting rooms and departments to be enjoyed by patients, families, carers, visitors and staff alike.
It has been an opportunity for artists, staff, community groups to create new works using flowers.
The collection aims to reflect the rich diversity, not just in the flowers that can be found in and around the hospital, but the people and staff who will use and work in the new facility.
Three local arts organisations, Plantation Productions, Art in Hospital and Govan Youth Café, were asked to work with older people, young people and people with different cultural backgrounds living in the Southside of Glasgow.
There was an Open Call enabling anyone to propose a work for the Collection, and also three artists were commissioned to make groups of work for the Collection.
The 100 Flowers Project has been developed in partnership with Glasgow Life, the Hunterian Museum and Art Gallery and the CCA.
There will be a book published of all the works in the Collection, available for purchase in the Hospitals and in City museums, arts centres and shops. In addition NSGH Staff will be able to request that reproductions of the pictures from the 100 Flowers Collection are hung in areas that they work.
100 Flowers workshop in Govan, Govan Youth Cafe
James Winnett, Part of the 100 Flowers Collection. Photograph Tom Littlewood
A film of the 100 Flowers Collection can be viewed below or please click on the following links to view the collection in full:
Image set 1 / Image set 2 / Image set 3 / Image set 4 / Image set 5
Jephson Robb and Peter Richardson of ZM Architecture have designed three Pavilions and two bicycle shelters. All the structures reinforce the external way finding strategy being placed as key landmarks. The structures benefitted from significant additional funding from the Yorkhill Children’s Charity.
The Pavilions and Shelters are positioned as stopping points on journeys. Just going into hospital for an outpatient appointment or to visit someone can be stressful. The Pavilions and Shelters support that journey. When you sit in one of these pavilions and shelters and look up, day or night, you’ll see the pattern of the night sky. For a moment, you’ll be transported from your everyday context to somewhere magical.
When children visit the pavilion in the Children’s Park they’ll find a performance space where they can take the limelight. A spotlight on sensor activation will put them centre stage. Parents and carers can watch their children invent new stories or moves.
The two bike shelters and Garden and Play pavilions will be erected during 2015 with the final Orchard Pavilion planned for 2016.
Jephson Robb and ZM Architecture, Bicycle shelters in fabrication at M&S Steel. Photograph Mike Bolam
Jephson Robb and ZM Architecture, Bicycle shelters in fabrication at M&S Steel. Photograph Mike Bolam
Spinning Gold – Art and Architecture Programme
Context
The redeveloped Maternity Unit and new Neonatal extension within SGH campus brings together for the first time in Glasgow, Neonatal, Medical and Surgical Intensive Care. The facility will include a new state-of-the-art labour suite and two obstetric theatres plus a separate Fetal Medicine department, providing specialist diagnostic facilities and treatment to unborn babies.
The art and architecture programme for the Southern General Maternity unit was commissioned in October 2008 during the final stages of completion of the new Neonatal extension. Lead Artist partnership Koan3 worked in collaboration with an Art & Therapeutic Design sub management group – including Neonatal clinicians, Maternity staff and a key Planning manager- set up within the management structure of the Maternity Project Board. Koan3 also liaised with the project architect in developing a colour logic for the internal spaces to aide wayfinding throughout the new Neonatal building.
Concept
The conceptual approach and subsequent art projects were in the most part, shaped by the invaluable input received during ‘drop in’ sessions organised for staff and service users to give feedback, thoughts and suggestions on what they felt was essential in creating a therapeutic environment which would enhance the individual experience of the maternity environment.
‘The Journey’ emerged as a key underlying theme for the ‘Spinning Gold’ art programme which encompassed both the physical and emotional aspects of the Maternity experience within the building. From the mother’s arrival pre delivery to waiting to be admitted, her migration through the building to getting settled and prepared to give birth.
Koan3 identified key zones on this route which presented opportunities for artworks to provide a more personal and reassuring environment; helping to reduce confusion and anxiety by improving the individual experience of arrival, wayfinding and waiting for service users. The artworks make subtle references to nature and the celebration of life.
Spinning Gold – art programme in progress
Five artists were selected and appointed through an application process led by Koan3. Each undertook a project plotted along the Maternity ‘route’ within the unit as follows:
Main Maternity Entrance Artworks
Commissioned Artist:
The Flowerers – takes inspiration from the exquisite embroidery of the Ayrshire muslin ‘Flowerers’. Their use of symbols of purity and elegance is given a contemporary twist through the use of colour and modular patterns created solely by intersecting circles produced on translucent glazing film.
Meadow Wall -seven individual hexagonal wooden panels wall mounted opposite the reception area and aligned with each other in keeping with the flowerers modular pattern.
Lobby Access Lift Areas Artwork : Petals
Commissioned Artist:
Petals –The ceiling artwork uses natural geometries to form a visual language that balances femininity with science. A collection of three – dimensional ‘petal’ forms which are derived from a basic hexagon, each rotates in six directions to form a seemingly random scattering which encourages the eye along the route connecting to the main corridor.
Main Maternity Corridor Artwork: Colour Sentences
Commissioned Artist:
Colour Sentences – is a linear installation of shallow lightboxes which layer delicate plant imagery with sequenced ‘bands’ of developing colour to draw the eye along the main Maternity Corridor emphasising the transitional nature of this space.
Maternity Night Entrance: Strands
Commissioned Artist: Tony Stallard
Strands – a site-specific light sculpture in neon, designed to suggest DNA or RNA strands connecting the space, this ‘joining’ or ‘coupling’ by way of ‘strands’ suggest a symbolic reference to the biological link between Mother and child as well as the physical linking of spaces between the Maternity buildings in an architectural sense.
Neonatal Waiting Rooms: River of Names ( interactive Digital)
Commissioned Artist: Nicola Gear
River of Names – an interactive digital artwork for the monitors in the Neonatal waiting rooms. Visitors are able to touch the image of flowing water on the screens to hear the voices of local people telling stories and sharing memories surrounding the subject of naming a child.
Neonatal Main stairwell : Sonar Landscapes
Lead Artist: Koan3
Sonar Landscapes is intended as a wayfinding artwork which ‘flows down through all three floors of the Neonatal unit stairwell. Each section houses a small portal window at the centre, softly lit and encompassing a miniature landscape themed to correspond to the level of energy and emotion on that particular floor.
Neonatal Roof Terrace: Garden of Contemplation
Lead Artist: Koan3
Garden of Contemplation – an ornamental ‘viewing garden’ on the roof terrace over looked by the Special Care Baby Unit and potentially the new Children’s Hospital. The design focuses on a contemplative space, which incorporates visual poetry/typography etched onto delicately coloured glass panels; intended to evoke pauses in time and moments captured between thoughts it offers a peaceful focus for visitors.
Lead Artist Curator: Koan3 (Artists Callum Sinclair & Lorraine Aaron)
Architects: Hypostyle
Funders: Grant funding £200,000 received from Yorkhill Children’s Foundation
Contributions from Women & Children’s Directorate
Key Dates: Appointment of Lead Artist – Oct 2008
Art programme Install begins – July 2010
Expected Completion – Most artworks by Oct 2011
Two projects affected by Maternity Refurb timeline.
An MSK (musculoskeletal) physiotherapist can provide expert assessment and advice to help you manage pain, disability and injury to your joints, muscles or spine.
We do this through questioning and physical assessment.
We want to know what impact these problems are having on your life. Together we will discuss ways we can help aid your recovery and guide you to achieve your goals.
We can assist in helping you:
MSK Physiotherapy may not help if you:
This What Happens Next leaflet explains what will happen once we receive your referral.
The Patient Information About Your Appointment With a Musculoskeletal Physiotherapist leaflet will give you more detail about what to consider and expect once an appointment has been arranged.
We know that many musculoskeletal (MSK) conditions benefit from good self-care and self-management. Use the icons below to link to information, videos and leaflets that you may find helpful. You can use this information independently or after receiving a diagnosis from a health professional. Please note that all the resources on this site are aimed at individuals aged 14 and over.
If you can’t find what you are looking for on this page you can also visit NHS inform for other resources.
We want to make these pages as helpful as possible. Your feedback will really help us to improve the parts that matter most to you. The short, confidential questionnaire should take about 2 minutes to complete.
We are always trying to improve and would value your feedback about the physiotherapy treatment you have received. This includes making a formal complaint.
Health Improvement describes our work to improve the health and wellbeing of individuals or communities through enabling and encouraging healthy choices as well as addressing underlying determinants of health such as poverty and lack of educational opportunities. We work with a wide range of partners to influence policy, service provision and wider environmental factors that help support positive health outcomes for our population, especially those in greatest need.
You can contact the Health Improvement team at:
ggc.health.improvement@nhs.scot
The decontamination of near patient equipment and medical devices is crucial to the prevention of healthcare associated infection (HAI). In recent years the Scottish Government have issued guidance and Health Department Letters to provide NHS Boards with information to ensure that this type of equipment is dealt with in line with current standards and guidance.
This page is divided into sections to ensure that staff with a direct responsibility for particular equipment, have the most up-to-date information and training available. Decontamination practice is continually evolving and those with a responsibility for decontamination need to ensure that they are aware of current developments.
If you require advice from the Decontamination Sub-Group please complete the attached Advice Request Form and return to ggc.infectioncontroldecontamination@ggc.scot.nhs.uk.
This document has been prepared to provide guidance on the technical requirements for the decontamination of flexible endoscopes and the options available. The document is intended to summarise key information on best practice in a manner which is readily accessible to the user/manager.
This guidance has been prepared by utilising published guidance from expert bodies, existing best practice guidance and standards, both published and in draft form. Many of the referenced standards are harmonised standards in respect of the Medical Device Directive.
Caused by unconventional agents thought to be infectious proteins – known as prions. Disease in humans are:
There is evidence that these disorders can be transmitted in specific situations associated with medical interventions, e.g. transfusion of contaminated blood and blood products, surgery with contaminated instruments. During routine clinical care, Standard Precautions are sufficient to prevent cross-infection in healthcare settings. Transmission Based Precautions must be applied when operations or specific invasive procedures are to be undertaken on high-risk tissues or patients identified as being at risk of vCJD.
Guidance from the ACDP TSE Risk Management Subgroup (formerly TSE Working Group) is the most-up-to date guidance on this topic, provided by the Department of Health.
See also the NHSGCC CJD SOP.
Hand Hygiene is one of the most effective actions to reduce the spread of pathogens and prevent infections, including the COVID-19 virus. Conducting hand hygiene at the right time, using the right technique, with either Alcohol-Based Hand Rub (ABHR) or soap, water and disposable towels is critical.
All healthcare staff should follow the National Infection Prevention and Control Manual to prevent spreading infection to those in the healthcare setting.
Members of the public can help prevent infections when visiting healthcare settings by following the advice in our Healthcare Associated Infection: Information for the public leaflet.
Further information about the global campaign led by the World health Organisation can be found on the WHO website.
Contact Name: Stefan Morton, LHBC, Infection Prevention and Control
Email: stefan.morton@nhs.scot
Our poster and video demonstrates the 5 moments of hand hygiene.
Infection Prevention and Control (IPC) staff collaborated to produce an informational video regarding 5 Moments of Hand Hygiene. This was developed to highlight the common failures that medical staff incur, as reported in audits of compliance. The video also highlights various anecdotal responses when challenged, given by existing medical staff members within NHSGGC. It features an introduction and closing statement by David Stewart, Lead Director for Acute Medical Services.
Staff involved in making this video were recruited from the North East IPC Team and Glasgow Royal Infirmary (GRI). Recording and post-production was carried out by GRI Medical Illustrations.
Please click on the links below to view the NHS Greater Glasgow and Clyde Hand Hygiene Videos. The videos are best viewed with sound on.
Infection Control training modules, including those offered by NES, can be accessed via learnPro.
Hand Hygiene audits should be carried out on a monthly basis within NHSGGC wards and departments. The audit tool should be utilised in conjunction with the information contained in the documents. The audit should not be carried out by the SCN as awareness of senior staff can change practice in clinical areas. 2-3 auditors should be chosen from a mixture of grades, including Bands 5 and 6 and HCSWs.
The data gathered should then be uploaded to the CAIR Dashboard.
Please note, exactly 20 observations must be recorded to complete an audit; any more or less will result in an error.
For further information regarding this process, please contact Stefan.morton@nhs.scot
Hand Hygiene Aide Memoire (new document)
NHSGGC’s Arts and Health initiatives foster safe, welcoming environments and enhance the healthcare experience for patients, staff, and visitors. Through a person-centred and integrated approach, the programme leverages the positive impact of art, architecture, design, music, and nature on health and wellbeing.
Programmes are evidence-based and include public art commissions, creative workshops, and integrated design strategies across clinical buildings and green spaces. Developed in collaboration with artists, educators, voluntary sector organisations, and funders, the work celebrates Scotland’s creative talent.
Explore the programme highlights below, including innovative designs for clinical spaces and the role of arts in healthcare.
The Arts and Health programme contributes to reducing health inequalities by improving access to the arts. It enhances care environments, supports treatment, and sparks dialogue that informs service improvement. Community-based creative health projects foster collaboration and strengthen local relationships.
Located at the Princess Royal Maternity Hospital, this mural responds to campaigner Rachel Dallas’s work on maternal health inequalities. It has prompted meaningful conversations and cultural change within NHSGGC.
“It’s not just a mural”
Read more about the project here: Work completes on giant mural at Glasgow Royal Infirmary
Click on the image below to view our Arts and Social Justice gallery on Flickr.

This innovative programme brings performing arts, exhibitions, and artist residencies into healthcare settings, demonstrating the psychological and physiological benefits of cultural engagement. It provides opportunities for artists and partners to showcase work in clinical environments, often offering patients their only access to the arts.

Art is integrated into the design and enhancement of green spaces, promoting outdoor activity and wellbeing. Programmes span clinical and mental health sites and extend into neighbouring community areas.

Alec Finlay’s sculpture marks the entrance to New Stobhill Hospital, encouraging interaction with nature through poetry-engraved boulders, bird boxes, and seating. This project broadened architectural thinking to include surrounding landscapes.
At Gartnavel Royal Hospital, this long-standing initiative supports mental health recovery through exhibitions, public art, and green space activities. Inspired by patient creativity, it is sustained by volunteers and partnerships with organisations like Common Wheel and Project Ability.
The programme has influenced similar initiatives at Leverndale and Stobhill Hospitals.
Click on the image below to view our Art and Green Spaces gallery on Flickr.

This strand modernises healthcare environments through integrated art and design in new builds and refurbishments. Artists collaborate with architects and stakeholders to create therapeutic spaces.
Part of the South Glasgow University Hospital development, this project enhanced over 80 quiet rooms using biophilic design principles to support sensitive conversations.
Find out more: https://www.nicolamurray.com/work/case-studies/nsgh-dignified-spaces/
https://www.artinscotland.tv/2015/dignified-spaces-project/
Curated by Clare Phillips for Ginkgo Projects, this collection features works by over 70 artists and is installed throughout the new hospital buildings.

Art in Hospital delivers a comprehensive visual arts programme across Glasgow and Scotland. Initially focused on older adults in long-term care, it now supports a wide range of patients, including those in rehabilitation, palliative care, and mental health services. The programme promotes wellbeing and self-expression through creative engagement.
Creative and performing arts have a proven impact on health and wellbeing. NHSGGC’s programmes bring together professional artists and community organisations across diverse media including drawing and painting, printmaking, photography, textiles, video, dance, music and drama.
Explore more about our initiatives, partners, and research through the links below.
The Buddy Beat
A Renfrewshire drumming group for adults with mental health experience, aimed at promoting social inclusion and helping people self-manage their week.
Culture Health & Wellbeing Alliance
Arts, Culture, Health & Wellbeing, Scotland (ACHWS)
ACHWS has developed into an active Scotland-wide network providing information and support for anyone working across arts and culture, health and wellbeing. It is a collective voice for arts and health in Scotland.
MacDonald, Raymond AR (2013)
Music, health and wellbeing: a review International Journal of Qualitative Studies in Health and Wellbeing
Common Wheel A charity that supports people managing or recovering from mental illness and dementia by providing meaningful activities.
Scottish Health Equity Research Unit (SHERU)
Leave No One Behind (2023) Report on the state of health and health inequalities in Scotland: https://www.health.org.uk/sites/default/files/upload/publications/2023/HF_Health_Scotland_Web_Final.pdf
Project Ability Creating opportunities through inclusive art for all, providing a welcoming arts community for people with learning disabilities and mental ill-health.
Glasgow Medical Humanities Network
Scottish Mental Health Arts Festival
British Association of Art Therapists
Evidence summary for policy: The role of arts in improving health and wellbeing (2020)
Creative Scotland Arts and Health Map (2021) https://www.creativescotland.com/binaries/content/assets/creative-scotland/resources-and-publications/research/2022/creative-scotland-arts-and-health-mapping-report.pdf