Frequently Asked Questions
How do I get access to the TURAS Appraisal system?
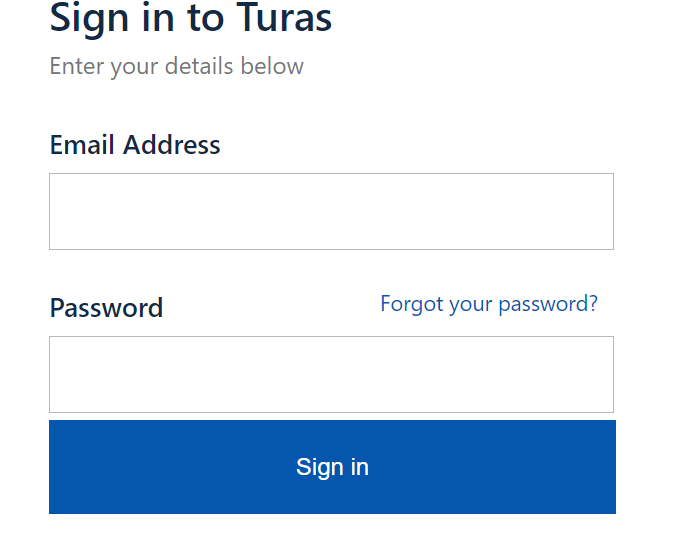
If you have previously logged on to your account and have forgotten your password you can reset it using the “Forgotten your Password?” link on the sign in page.
This quick guide gives information on the process for new staff. If you are a new user and you don’t have a username or password, please speak to your line manager who will contact Learning and Education to get you added to their TURAS Appraisal managers page and request a username and password for you. This will be issued by Learning and Education, direct to you, by e-mail.
I don’t see TURAS Appraisal when I login to my TURAS Account – why not?
You can’t add TURAS Appraisal into an existing TURAS account yourself. If you contact the Learning and Education Support Team via NHS Service Now or call 0141 278 2700 option 3 they will provide login details for your TURAS Appraisal account. You can continue with separate login details for your different TURAS applications or L&E Support will advise how you can get the National Digital Team to merge your accounts so that you have the one login for all TURAS applications.
Not all the staff are listed on my managers page that should be. How do I add staff?
To add staff to your Turas Appraisal account please complete the Staff List Template and send this to Learning and Education Support Unit via NHS Service Now.
The form has to be completed by the manager/PA only, not the staff member. Only new or missing staff are to be added to the form, existing staff members should not be put on.
I need to allocate some of the staff on my managers page to other people in my team to carry out their review – how do I do this?
You can easily do this from your managers page.
See the user guide for instructions: How to Assign KSF Post Outlines and Reviewers to Staff
I need to allocate new/different post outlines to some of the staff on my managers page – how do I do this?
You can easily do this from your managers page. See the user guide for instructions: How to Assign KSF Post Outlines and Reviewers to Staff
I’ve Retired and Returned and my TURAS Appraisal has all changed – what do I do?
The information relating to your previous posts is still visible to you however if you had staff assigned to you this will need to be updated. This quick guide gives information on what you need to do.
How can I access my teams progress reports to check compliance?
TURAS Appraisal now has live Team Progress Dashboards. Both managers and reviewers will be able to view live information for the staff that they have assigned to them on TURAS Appraisal including the compliance percentage of signed off reviews, status of reviews, information on PDPs, objectives and also a to do list where there are outstanding actions. Users guides below:
I know work is happening on Protected Learning Time and recording of it – How does it link to Personal Development Planning & Review and TURAS Appraisal?
Three National Workstreams have been established: 1) Core Training & Training Passport, 2) System modifications and 3) Measures. There is a working group at Board level in NHSGGC which links into these and takes forward the work. Further information is available on the Protected Learning Time Sharepoint page.
Additional Information
User Guides
To help you use and navigate TURAS Appraisal we have provided the following “How to” guides along with some other information:
- How to record PDP&R information – Reviewers
- How to record PDP&R information – Staff
- How to use the reviewer team progress dashboard
- How to use the manager team progress dashboard
- How to update personal details and add other Turas Applications
- How to assign a post outline and a reviewer
- TURAS Appraisal set up – Process for New Staff
- Guidance for Retire and Return staff
- Verifying your TURAS Appraisal Account
The guide below provides you with information about what to record on TURAS Appraisal and when you should record it: What to record and when.
Managers and Reviewers – TURAS Appraisal Account
Keeping your TURAS Appraisal account up to date
To add staff to your TURAS Appraisal account:
- Please complete the Staff List Template and forward this to the Learning and Education Support Team via the NHS Service Now Portal.
- The form has to be completed by the manager/PA only, not the staff member
- Only new or missing staff are to be added to the form, existing staff members should not be put on.
To remove staff from your TURAS Appraisal Account:
- If the member of staff is leaving NHSGGC completely – No action is required. Once terminated from the Payroll system they will automatically be deleted from TURAS Appraisal
- If the member of staff is moving to another department – contact the Learning and Education Support Team via NHS Service Now providing the name and payroll number of the member of staff to be removed
Assigning reviewer rights to members of staff that you want to review members of your team:
- At this time only the Learning and Education Support Team can assign reviewer rights. To arrange this the manager of the person that reviewer rights is required for should contact the Learning and Education Support Team via NHS Service Now. Please provide name and payroll number of the person that reviewer rights is to be assigned to.
Assigning a reviewer and assigning/changing a KSF Post Outline for staff:
- Please see User Guide on how to assign a post outline and reviewer for further information.
Reports
Reports are available from the Team Progress Dashboard on your TURAS Appraisal account. If you have manager or Reviewer access to the system and have staff assigned to your account you will automatically have access to the dashboard.
The Team Progress report will give you live information on compliance rate for your team with regards to reviews, PDPs and objectives. It also has a to do list to alert you if any actions are required.
KSF Post Outline Information
Approved KSF Outlines in NHSGGC
This link will provide you with information on all KSF post outlines for NHSGGC staff. You will be able to view the title, pay band, all dimensions and levels included in the KSF post outline.
It does not included the level descriptions but you will find these in the documents below and also in the KSF handbook.
Occasionally there may be a KSF Post Outline on the spreadsheet that will not be on TURAS Appraisal. This is because on the day e-KSF was decommissioned the KSF Post Outline was not assigned to any members of staff, only KSF Post Outlines in use were migrated to TURAS Appraisal.
- C1: Communication – Levels 1-4
- C2: Personal and People Development – Levels 1-4
- C3: Health, Safety and Security – Levels 1-4
- C4: Service Improvement – Levels 1-4
- C5: Quality – Levels 1-4
- C6: Equality and Diversity – Levels 1-4
- G6: People Management – Levels 1-4
- How To Assign KSF Post Outlines and Reviewers on Turas Appraisal
Help and Support Contacts
Learning and Education Support Team
- NHS Service Now Portal – Click on the L&E Icon and fill in the relevant fields. You will receive an acknowledgement which will include a ticket number for your query. How to raise a query through NHS Service Now Portal.
- 0141 278 2700 (12700 internally) – choose option 3 for Learning and Education. Open 10.00am – 3.00pm, Monday to Friday
Please supply your GGC payroll number when you contact the team.