Your health
Staff Guidance & Policies
We have a range of guidance and policies which support diversity in the workforce. These include:
- Equality and Diversity Management Guidance
- Adoption and Fostering Policy
- Policy on Breastfeeding
- Flexible Working Policy
- Gender Based Violence Policy
- Maternity Leave Policy
- Parental Leave Policy
- Reduced Working Year Policy
- Special Leave Policy
- Equal Pay Statement
Support for Staff with Money Worries
In the current economic climate, many staff are experiencing money and debt problems, which can increase personal stress. NHSGGC has a number of resources to support staff.
Our All About Money page is specifically for staff and offers a wide range of help, practical support and advice.
Staff Forums
For more information visit our Staff Forums web page.
Staff Disability Forum
The Staff Disability Forum is the longest established staff forum. It aims to make positive changes in the organisation and provide a support network for disabled staff.
For further information visit their web page.
LGBTQ+ Staff Forum
For NHSGGC staff members who want to contribute to creating a more LGBTQ+ inclusive workplace, there is a LGBTQ+ forum. The Forum is a group of staff who identify as lesbian, gay, bisexual, transgender, queer inclusive (LGBTQ+), and allies.
The group aims to create a safe and welcoming space for staff members within our LGBTQ+ community, with social activities, a programme of events, and formal as well as informal meetings.
To join or for more information about the group, visit their web page.
Black & Minority Ethnic Staff Forum
This group has been formed as a result of discussions held with Black & Minority Ethnic staff about their experience of working in NHSGGC. Issues raised by staff included stereotyping, discrimination and organisational culture, as well as the impact of negative media reporting and the anti-immigration climate.
In addition to providing a support network for Black & Minority Ethnic staff, the Forum is supported by members of the Workforce Equalities Group to make positive changes within the organisation.
For further information, visit their web page.
Was this helpful?
Interpreting Services – British Sign Language (BSL) and Spoken Language Interpreters
It is the responsibility of NHSGGC staff to provide an interpreter for patients attending any of our healthcare services.
Please note that the provision of interpreters is paid for directly by the NHSGGC interpreting service. There will be no cost to your local service for this.
For more information on this service, go to HR Connect/Interpreting
Booking a British Sign Language Interpreter (BSL)
NHSGGC has an ethical and legal responsibility to provide BSL interpreters to support effective and safe communication with Deaf patients who are BSL users.
It is important to note that family members should not be used as interpreters.
Interpreting support must be provided as follows –
· All services must book BSL Interpreters for any scheduled outpatient appointments where we know the patient requires this support.
· For an inpatient –
- on admission – planned or unplanned
- on transfer – between wards or Acute receiving to in-patient ward
- on discharge
- at doctors’ rounds – every day
- at significant nurse interventions
- for pre and post-surgery
- for the entire period of labour in Maternity
- for all ED assessments – including triage
· BSL Interpreting support must also be provided at least once per day for Deaf BSL inpatients to allow questions and answers regarding their care.
· Out with this time, Deaf BSL inpatients must have access to BSL Online interpreting support for any care needs that arise. Do not make assumptions about how well a Deaf BSL patient understands spoken or written communication. Information could be missed or misunderstood and the patient put at risk.
· Where a BSL interpreter is unavailable or the situation is unplanned or an emergency, staff must access BSL online interpreting support. The BSL Online service can be easily accessed by any available device, such as the ward iPad or any mobile phone, using the QR code.
If you are aware of any barriers that might restrict the use of BSL Interpreting in your patient area, we want to hear from you. Please contact us.
Out of Hours Procedures
NHSGGC Interpreting Service (8.00am until 6.00pm Monday to Friday, 8.00am until 4.00pm Saturday to Sunday)
E-mail: interpretingservice@ggc.scot.nhs.uk
Telephone: 0141 347 8811
Outwith these hours, please contact the patient’s preferred agency, if provided, or call 0141 347 8811 to be connected to an appropriate service.
You can also access the BSL Online Interpreting Service which is available 24/7.This service allows staff to communicate with Deaf BSL patients while waiting for a face to face interpreter to arrive.
Telephone Interpreting
Telephone interpreting is available 24/7 and can be accessed by calling or using the app.
For more information on this service, go to HR Connect/Interpreting
Direct Patient Access Telephone Interpreting
Patients can now access the telephone interpreting service to contact any NHS Greater Glasgow & Clyde service.
For example, patients can use the telephone interpreting service to call from home and make an appointment with their GP, discuss medications with their Pharmacy or book a Maternity appointment.
An information leaflet is available in multiple languages. It explains how to use the service by calling or by using a mobile app and provides patient codes specific to NHSGGC services.
Booking a Face to Face Interpreter
Contact NHSGGC Interpreting Service (8.00am – 6.00pm Monday to Friday, 8.00am – 4.00pm, Saturday to Sunday)
Email: interpretingservice@ggc.scot.nhs.uk
Telephone: 0141 347 8811
Out of Hours Procedures
Call 0141 347 8811 to be connected to the appropriate service.
Additional Resources
- NHSGGC Interpreting, Communication Support & Translation Policy
- How to Access Interpreting Support Wall Chart
- Language identification poster
- Language identification leaflet
- Accessing British Sign Language Support – Staff leaflet
- NHSGGC Interpreting Quick Guide
Printed copies of the above are available from equality@ggc.scot.nhs.uk
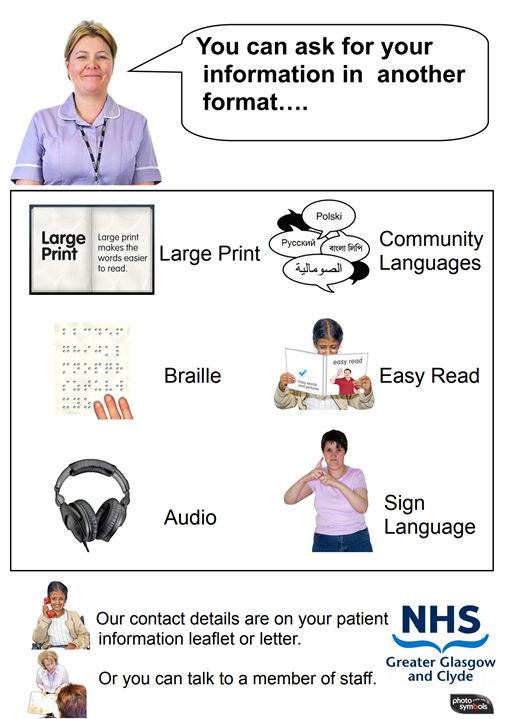
Alternative Format / Language Text
As a statutory organisation, we are required to provide information in a format which all our service users can understand. This includes providing information in accessible formats such as audio, Braille, large print and community languages.
Every time a new piece of information is produced or an existing one reviewed, it should at the same time be produced in audio CD, words and pictures, Braille, large print, British Sign Language DVD and in our top five spoken languages (review annually).
We must also respond to any individual patient request for information in any accessible format or language of their choice.
A statement has been produced that should be placed in all leaflets. It states the following in English plus the ‘top six’ community languages (currently Polish, Mandarin, Romanian, Arabic, Urdu and Farsi).
‘If you require this information in an accessible format, such as large print or braille, or in a community language, please use the contact details on your patient information leaflet or letter.’
Ordering as an insert
This insert should be included with appointment letters and pre-attendance information posted to the patient, and can be given to patients on attendance at clinics or on admission. It is supported by posters displayed within hospitals and GP surgeries and is also offered on Solus Screens.
The leaflet is available from stock in packs of 100 and can be ordered via the PECOS system or by any method used to order goods from stock (e.g. paper indent). It is available in 2 formats to suit varying distribution methods – as a single sided A5 sheet or as a one-third A4 sheet (compliments slip format) suitable for DL type envelopes.
Order codes are as follows:
- 97106 – Size 1/3 A4 (compliments slip format)
- 97107 – Size A5
Printing the statement within a publication
If you would like to include the statement in your document (as opposed to using an insert), you can use image 1 (portrait) or image 2 (landscape) and adjust to size.
Other formats
This statement is also available in other formats, including words and pictures, audio and British Sign Language.
Producing Accessible Patient Information – other formats and languages
NHS Greater Glasgow and Clyde (NHSGGC) produces vast amounts of information. The task of making this information accessible to all is a significant challenge but is vitally important in ensuring every patient fully understands and can be involved in the care they are receiving.
The purpose of our ‘Clear to All’ Accessible Information Policy is to make sure there is a consistent, accurate and clear approach to providing accessible information to patients and members of the public.
Information can be produced in the format that best meets the patient’s needs. For example, this could be large print, easy read, audio or braille. It can also be translated into any spoken language and British Sign Language.
Requesting translations and other formats
Information in other languages or formats can be accessed via the Clear to All service.
Staff Resources
Step by Step Staff Guide to Producing Accessible Information
Informing Patients of Right to Alternative Format/Language inserts – see Alternative Formats/Languages section above.
Language Identification Card (PDF)
Patient Information
These resources provide the following statement:
‘If you require this information in an accessible format, such as large print or braille, or in a community language, please use the contact details on your patient information leaflet or letter.’
Multi-language version (PDF)
Audio version (MP3)
Words and pictures version – English (PDF)
Words and pictures version – Arabic (PDF)
Words and pictures version – Simplified Chinese (PDF)
Words and pictures version – Polish (PDF)
Was this helpful?
Age
Disability
- NHSGGC Assistance Dog Policy (Review 2022)
- NHSGGC BSL National Plan (2024-2030)
- Disability Perceptions Gap
- NHSGGC Health Needs Assessment – Deafblind and Deaf Communities
- NHSGGC Staff Guidelines for people who are Deaf, have hearing loss or are deafblind
- NHSGGC Staff Guidelines – Working with people with visual impairment
- Principles of Inclusive Communication – Scottish Government
- NHSGGC Powered Wheelchair Scooter Use Guidelines
Gender-Based Violence
Gender Reassignment
Supreme Court Ruling Update – Thursday 17th April 2025
We are currently reviewing our policies in light of the Supreme Court’s ruling on 16 April 2025 that ‘sex’ in the Equality Act 2010 refers to biological sex.
- NHSGGC Transitioning in the Workplace – Guidance for Managers Nov 24 (under review)
- Changing Your CHI (under review)
- Gender Reassignment Policy Review 2021 (under review)
- Sharing Trans Information (under review)
General
- Clear to All Accessible Information Policy 2021
- NHSGGC Interpreting, Communication Support and Translation Policy
- Equality Law – A Manager’s guide to Getting it Right in NHSGGC
- Equality Monitoring Form – 2024 version
- Examples of projects to prevent and reduce violence in Scotland
- Exploring the Cost of the Pregnancy Pathway
- Human Rights Based Approach in NHS – literature review
- Is Scotland Fairer? Equality & Human Rights Commission
- Maximising the role of NHS Scotland in Reducing Health Inequalities
- Models of Incorporation and Justiciability for Economic, Social and Cultural Rights
- Patient Public Health Information Management Policy 2021
- Public Health Reform – Scotland’s Public Health Priorities
- NHS Greater Glasgow & Clyde Mitigation Guide – September 2023
Hate Crime
Race & Ethnicity
Religion & Belief
- A Multi-Faith Resource for Healthcare Staff
- Advice to British Hajjis
- Faith and Belief Communities Manual
- Information and Guidance on Visiting Hospitals for Faith and Belief Community Representatives
- Ramadan Health Guide
- Seen and Not Heard – Voices of Young British Muslims
- Spiritual Care Policy
- Values in Harmony
Sex
- A Guide to Support Services for Children and Young People Experiencing Domestic Abuse in West Dunbartonshire
- Ethnic Survivors Forum
- Everyday Terrorism: How Fear Works in Domestic Abuse
- Facts for Fathers-to-be
- Human Trafficking – Making the links
- Older Women and Work: Looking to the Future
- Women – Where to go for advice, support and information in the Glasgow area
- Women Living with Domestic Abuse in West Dunbartonshire
Sexual Orientation
- National LGBT+ Health Needs Assessment 2022 – short films explaining the process and outcomes – Full summary of findings Wish list
- Don’t look back?
- Fair For All – The Wider Challenge – Good LGBT Practice in the NHS
- Gay and Bisexual Men’s Health Survey Scotland
- Getting Equalities Monitoring Right
- Halt Hate Crime
- Hate Crime – What You Need To Know
- Hate Crime Poster
- Hidden Lives
- Inclusive Language in the NHS
- LGBT In Scotland – Health Report
- Life in Scotland for LGBT Young People
- Not Just A Friend
- Protecting Patients – Your rights as LGB people
- Social context of LGBT people’s drinking in Scotland
- Tackling Homophobia
- The Needs and Experiences of LGBT People in Glasgow
- Your Services, Your Say
Was this helpful?
Martin is a Deaf man whose first language is British Sign Language. A smoker for many years, Martin finally decided to take the plunge and quit. After looking at the various options available to help him, he decided that he would like the support of a group. On enquiring, however, Martin was told that he could not attend a smoking cessation group because there was no budget for an interpreter.
This is a real example of discrimination which happened in NHSGGC. It was our responsibility to ensure Martin could use this service. To meet our patient commitment, and by law, a BSL interpreter should have been made available.
This section provides real examples of how people have been affected by discrimination within NHSGGC. It highlights the training and resources available to staff to help us treat people fairly. It also looks at what’s being done to ensure a working environment for staff which is free from harassment or discrimination of any nature.
What is Discrimination?
We discriminate when we treat people as if they are all the same even when they have different needs. We also discriminate if we treat people differently in a negative way based on their gender, age, social class, sexual orientation, race, faith & belief or disability.
Every one of us has to be aware of and tackle discrimination. Not only should we want to ensure that patients get the services they need, we should be aware that by law we must not discriminate either against patients or staff members.
People’s Experiences
Jelina
Jelina is an older Pakistani woman who cannot speak English or read in any language. Jelina was admitted to hospital for a stay of several weeks.
During this time, staff did not communicate with her and she was left completely isolated in her already vulnerable state. Jelina’s family had to draw pictures for her to use to make very simple requests.
What should have happened?
Jelina’s communication needs should have been assessed immediately so that support could have been provided for both her and the staff. This support may have taken the form of an interpreter and/or language assistance materials.
Julie
Julie is a 34 year old gay woman whose partner is terminally ill. During a hospital visit, Julie was asked not to show affection to her partner because it was making the other patients feel uncomfortable.
What should have happened?
It was wrong to discriminate against this couple on the basis of their sexual orientation. Julie and her partner obviously wanted to be able to comfort each other at this difficult time in their lives and should have been treated as any other couple.
Tina
Tina Watson is a transgender woman. She visited an NHS clinic, and when called from the waiting room was referred to as Stephen Watson – her former name. Tina approached the desk and explained that her name was not Stephen and that she should be referred to as Tina or Ms. Watson. The receptionist stated that they would continue to use the name on his records until he presented a new passport.
What should have happened?
Tina should have been treated in the same way as any other patient amending their personal details. For transgender people this is particularly sensitive and it is our responsibility to ensure records are amended. In this case, where there had clearly been a breakdown in communication, the receptionist should have apologised for the mistake, addressed the patient as requested and ensured that the paperwork was updated.
Charlotte
Charlotte and her husband are asylum seekers from Africa. Pregnant with her 4th child, Charlotte attended the maternity services in her local hospital.
After a smooth pregnancy, Charlotte gave birth to a healthy baby boy. Prior to discharge from the hospital, Charlotte was given information about contraception. This is common practice. However, the midwife introduced the subject by saying, “We don’t want you coming back here every year – you need to do something about this.” Charlotte at first thought that she was joking but quickly realised she was serious. Shocked, she described the approach of the midwife as ‘provocative’.
What should have happened?
The comment made to Charlotte was clearly based on the midwife’s own assumptions about her circumstances. The implication that Charlotte’s family was the result of thoughtlessness or ignorance, or that Charlotte and her husband would not want more children, was presumptuous and insulting. The contraception advice should have been offered in a friendly, informative manner. An open approach would have allowed the patient to disclose any particular concerns.
John
John is both visually and hearing impaired. He faces a range of obstacles every time he attends services. Firstly, he finds it difficult to read the correspondence he receives about appointments. This means he has to rely on someone else reading what can often be personal, private information. When attending an appointment, he can’t hear when his name is called out and, on one occasion, despite alerting staff to his situation, missed his appointment completely.
John uses the support of a guide/communicator for any regular appointments or hospital stays. However, during a recent admission, staff went ahead with a procedure after his communicator had been asked to leave. With no way of knowing what was happening or why, John was extremely distressed by this traumatic situation.
What should have happened?
John should have been asked what could be done to make written information accessible to him. Letters should then have been sent to him in an appropriate format, e.g. large print. Noting John’s communication needs in his file would have informed staff of the right steps to take. Similarly, if staff had been aware of his hearing impairment, then they would have understood the need to go and get John in the waiting room, rather than calling out.
Everyone is different, and by talking to John through his communicator his communication needs could have been assessed and acted on. For example, staff may have been able to communicate with him in an emergency by learning the deafblind alphabet and putting a poster behind his bed.
Was this helpful?
Scottish Child Payment is now open for applications
Scottish Child Payment is a new payment for families on tax credits or certain benefits to help towards the costs of looking after a child. It is £40 paid every four weeks for each child under six.
The payment starts on Monday 15 February 2021, with first payments made from the end of February onwards, but Social Security Scotland is taking applications now to help manage demand.
You can apply if your child will be under six on 15 February 2021.
The qualifying benefits are:
* Child Tax Credit
* Income Support
* Pension Credit
* Working Tax Credit
* Universal Credit
* Income-based Jobseeker’s Allowance (JSA)
* Income-related Employment and Support Allowance (ESA)
Social Security Scotland will ask for evidence that the person applying is responsible for a child under six, usually through the child being named on a benefit claim form.
If more than one person applies for the same child, there’s a process for deciding who gets the payment – prioritising the person who the child lives with most of the time.
Scottish Child Payment will not be taken into account for UK benefit and tax credit assessments and there is no cap on the amount of children this payment can support.
First payments will be made from late February onwards. When someone gets paid will depend on how many applications we get and the process each individual application goes through.
If someone applied before Monday 15 February 2021, this will be the date that their
payment will be calculated from. If they apply after this date, it will be calculated from the date that they applied.
Payments will be made every four weeks following the first payment.
Find out more information and apply at mygov.scot/scottish-child-payment or call Social Security Scotland on 0800 182 2222.
Was this helpful?
PIP is a new benefit for people aged 16-64 who have a disability, physical impairment or mental health condition.
It will replace Disability Living Allowance (DLA) but more people will qualify for PIP than DLA.
PIP aims to support people that are experiencing difficulties with daily activities and mobility that are likely to last for 12 months or more.
We want to ensure that patients who have problems with daily living, such as eating or preparing food, taking medication, moving around or managing money, are aware of this benefit and how to claim it.
Posters and leaflets promoting PIP have been produced by NHSGGC and are being distributed throughout our services.
Get In Touch for more information.
NHS Greater Glasgow & Clyde have put in place a range of initiatives on money worries and employment which can make a substantial difference to vulnerable patients and families. For more information click here.
Was this helpful?
Person centred care is at the heart of the National Quality Strategy and aims to deliver effective, safe, non-discriminatory and efficient health and social care.
Being sensitive to inequalities and human rights within person-centred care means working in a way which responds to the life circumstances that affect people’s health. Evidence shows that if these issues are not taken into account by the health service, opportunities are missed to improve health and to reduce health inequalities.
Current Areas of Work
Our Frontline Equality Assessment Tool (FEAT) programme is being expanded to deliver a range of reviews across both Health & Social Care Partnerships and our Acute services in 2025/26. The programme offers a sense check which highlights both where there are gaps in services’ inequalities sensitive practice and where there are examples of good practice which could be replicated in other services.
Equality Impact Assessments (EQIAs) across the system are identifying areas for Disability Discrimination Act (DDA) or physical access audits aligned to the FEAT. NHSGGC has a duty to remove access barriers for disabled patients and these audits provide assessments of a physical environment with proposed enhancements reported back to our Estates and Facilities Directorate.
Our Anti-racism Plan aims to ensure that an anti-discriminatory approach to patient care is evident, particularly across key service areas such as Coronary Heart Disease, Type 2 Diabetes, Maternity and Mental Health. The Plan reflects our Equality Outcomes (2025 – 2029) and brings together our existing anti-racism work and our planned new activities in a single document.
Was this helpful?
NHSGGC wants to work in partnership with patients, learning from patients’ lived experiences.
We want to ensure that all voices are heard. The Equalities & Human Rights Team’s patient involvement activities therefore specifically engage with people with protected characteristics and other groups that experience discrimination.
People’s experience of inequalities and discrimination impact upon their health, how they engage with health services and manage their health problems. By engaging with communities and responding to feedback we can improve everyone’s experience of NHSGGC services. This work will also inform our equality outcomes and actions for the future.
The Equality and Human Rights Team also work closely with the Patient Experience Public Involvement Team to help reach and engage with all our communities.
Involving Patients and Members of the Public
We consult with a variety of patient groups depending on the area of work. For example –
Disability Access – our Disability Access Patient Group, help us investigate and audit the factors affecting disabled people’s access to our buildings and services.
Learning Disability – we work in partnership with a number of organisations supporting people with a learning disability and are members of The Life I Want Health Group, a partnership forum made up of 3rd sector (charitable) services. This engagement is vital in helping us improve experiences and health outcomes for patients with a learning disability.
Black and Minority Ethnic Communities – our engagement is constantly being developed and delivered with a range of charities working with BME communities. This informs our work to ensure communities have access to health information and that our services are delivered in ways which provides access for all. As such, it is an integral part of the ongoing development of our Anti-Racism Plan. For example, we have been working with the Minority Ethnic Carers of People Project (MECOPP) to better understand the needs of the Gypsy Traveller population within GGC, with the aim of improving access to health services, reducing stigma and discrimination and build trusting relationships.
The Deaf Community – feedback is sought from the Deaf community on a range of issues, including the BSL National Plan, our Interpreting services and access to NHSGGC services. The BSL Health Champions – volunteers from the Deaf BSL community – work with us to achieve this and group meetings are open to any Deaf BSL user who lives in the NHSGGC area. The group also has a Facebook page which is used to share information and to get feedback from the BSL community.
The role of Peer Workers
Peer workers are people who draw on their own experiences to help and support others in similar circumstances. Their lived experience enables them to connect in a meaningful way with those they are supporting.
The role of Engagement and Educational Peer Workers was introduced in NHSGGC in 2022. Our current work focuses on Immunisation, Screening, Poverty and aims to –
- Support the ongoing patient engagement within the vaccination and screening programmes; identify barriers to up-take and provide accurate, accessible information on vaccines and screening and wider NHSGGC services.
- Maximise the contact with communities who find it hard to engage with NHSGGC’s routine patient involvement activities and support them to do so.
- Engage with people living in poverty, discuss the help and support available and signpost as appropriate.
The Peer Workers run discussion sessions with their groups on issues relating to healthcare and people’s experience of using NHS services. They also provide information on the advice and support available to NHSGGC patients, particularly around help with financial hardship.
Useful Resources
Was this helpful?
Domestic abuse, rape and sexual assault, prostitution, child sexual abuse and other forms of gender-based violence cause immense pain and suffering and are a major public health issue. The emotional, psychological and physical consequences of gender-based violence can be profound and include fatal injury, physical health problems, chronic conditions, mental health problems and negative health behaviours.
Many people affected by gender-based violence are reluctant to disclose this experience, often through fear or shame. However, they do present across the whole range of primary and acute health settings. Health workers are therefore in a unique position to provide help and support. If we do not ask about or respond to gender-based violence there is a danger that the health issue won’t be treated properly and could increase the risk of long-term and chronic ill-health and even death.
Health workers across the whole of the health service need to know about gender-based violence, what to look for and how to respond. This is fundamental to our duty of care to patients and part of our role to promote gender equality.
The prevention of gender-based violence and the care of people experiencing it is a key priority for public protection within NHS Greater Glasgow and Clyde.
Key NHS Documents
- Gender-based Violence Policy Overview | NHS Scotland
- Gender-based Violence Guideline – Emergency Department and Minor Injuries Unit
Other Publications
- Equally Safe strategy – Violence against women and girls (VAWG) – gov.scot
- Adult Support and Protection: Guidance for General Practice, Scottish Government
- National-guidance-child-protection-scotland-2021-updated-2023.pdf
- Female Genital Mutilation (FGM) Multi-Agency Guidance, Scottish Government
- Scotland’s Trafficking and Exploitation Strategy 2025 – gov.scot
- Ending violence against women and girls: A public health approach
Useful Links
Public Protection
Commercial Sexual Exploitation
Domestic Abuse
- Domestic Abuse: Staying Safe, mygov.scot
- LGBT Domestic Abuse Scotland
- Men’s Advice Line UK
- Scottish Women’s Aid – changing attitudes, changing lives
- Domestic Abuse and Disclosure Scheme for Domestic Abuse in Scotland,Police Scotland
Prevention Campaigns
FGM and Forced Marriage
- FGM Aware, Women’s Support Project
- Scotland’s national action plan to prevent and eradicate FGM – gov.scot
- Forced Marriage, Scottish Government
Rape & Sexual Assault
- Archway Glasgow Sexual Assault Referral Centre, Sandyford
- Support after rape or sexual assault, mygov.scot
- Rape Crisis Scotland
Stalking
Trafficking for sexual exploitation
- TARA service for women trafficked for sexual exploitation, Glasgow City Council
- Encompass Network – support for women involved in prostitution
