For information on Trade Union and Professional Organisations and how to join, please select the relevant tile below.
Staff & Recruitment
The Employee Director is a Non-Executive Director member of NHS Greater Glasgow and Clyde (NHSGGC) and Co-Chair of the Area Partnership Forum. They work in partnership with the Board and its Executive Management to provide advice on workforce issues directly affecting NHS Greater Glasgow and Clyde. Working alongside the Employee Director are 2 Staff Partnership Leads and an APF Administrator.
Directly accountable to the Chairman of the Board and elected as the Chair of the Staff Side, the Employee Director and Employee Director’s Office is the Board’s conduit for 15 Trade Unions/Professional Organisations, and takes forward staff side views to influence Board Policies and to ensure that staff interests are properly reflected in Policy Development and encourage the ethos of Partnership Working.
Portraying positive behaviours and encouraging collaborative working, the Employee Director’s Office work with the Board to achieve its objectives and represent the views of NHS Greater Glasgow and Clyde staff by influencing debate and discussion.
To find out more about the Team and to access Trade Union/Professional Organisation or further information regarding the Area Partnership Forum (APF) and partnership working, please click on the tiles below.
The Team




More Information
Was this helpful?
If you require to speak with your Trade Union Lead or your local Staff Partnership Fora Staff Side Lead or Deputy Staff Side Lead, please see the contact lists below
Contact Details
Trade Union and Professional Organisation Leads
Contacts – Trade Union and Professional Organisational Leads
- British and Irish Orthoptists Society (BIOS), Vacant (please refer to the BIOS website)
- British Association of Occupational Therapists (BAOT), Amanda Jane Walton, AmandaJane.Walton@ggc.scot.nhs.uk
- British Dental Association (BDA), Vacant (please refer to the BDA website)
- British Dietetic Association (BDA), Simon Fevre, s.fevre@bda.uk.com
- British Medical Association (BMA), Scott Anderson, sanderson@bma.org.uk
- Chartered Society of Physiotherapy (CSP), Claire Ronald, ronaldc@csp.org.uk
- Federation of Clinical Scientists, Vacant (please refer to the FCS website)
- GMB, Karen Leonard, KL.Leonard@gmb.org.uk
- Hospital Consultants and Specialists Association (HCSA) , Allan Robertson, ARobertson@hcsa.com
- Royal College of Midwives, Emma Currer, emma.currer@rcm.org.uk (0300 303 0444)
- Royal College of Nursing, Barbara Sweeney, Barbara.Sweeney@rcn.org.uk
- Royal College of Podiatry (RCoP), Graham Pirie, graham.pirie@cop.org.uk (07825839336)
- Society of Radiographers (SoR), Christopher McGovern, christopher.mcgovern5@nhs.scot
- Unison, Frances Carmichael, fcarmichael@unisonglasgowclyde.com (07738803830)
- Unite the Union, Susan Walker, Unite the Union, susan.walker8@nhs.scot
Local Staff Partnership Fora Staff Side Leads and Deputies
A Staff Side Lead and Deputy Staff Side Lead is elected through the Employee Director’s Office on a 4 year term to represent the Area Partnership Forum at your local Staff Partnership Forum. If you are required to contact either, please see contact details below.
- Acute Partnership Forum
- Staff Side Lead – Frances Carmichael (Unison), fcarmichael@unisonglasgowclyde.com (07738803830)
- Deputy Staff Side Lead – Susan Walker (Unite the Union), Susan.Walker2@ggc.scot.nhs.uk (07724811532)
- Area Partnership Forum
- Admin Contact: Kirstin.McKenzie@ggc.scot.nhs.uk
- Clyde (Acute) Sector Staff Partnership Forum
- Staff Side Lead – Susan Walker, Unite the Union, Susan.Walker2@ggc.scot.nhs.uk ( 07724811532)
- Deputy Staff Side Lead – Margaret Duffy, Unison, mduffy@unisonglasgowclyde.com
- Diagnostics (Acute) Staff Partnership Forum
- Staff Side Lead – Susan Walker, Unite the Union, Susan.Walker2@ggc.scot.nhs.uk ( 07724811532)
- Deputy Staff Side Lead – Christopher McGovern, SoR, christopher.mcgovern5@nhs.scot
- East Dunbartonshire HSCP Staff Partnership Forum
- Staff Side Lead – Andrew McCready, Unite the Union, Andrew.Mccready@ggc.scot.nhs.uk (07479 658 758)
- Deputy Staff Side Lead – Vacant
- East Renfrewshire HSCP Staff Partnership Forum
- Staff Side Lead – Andrew McCready, Unite the Union, Andrew.Mccready@ggc.scot.nhs.uk (07479 658 758)
- Deputy Staff Side Lead – Marjorie Gaughan, Unison, Marjorie.Gaughan@ggc.scot.nhs.uk (07825 703606)
- Estates and Facilities Staff Partnership Forum
- Staff Side Lead – Rose Anderson, Unison, randerson@unisonglasgowclyde.com
- Deputy Staff Side Lead – Vacant
- Glasgow City HSCP Staff Partnership Forum
- Staff Side Lead – Josh Cairns, Unison, jcairns@unisonglasgowclyde.com (Phone – 07557796275)
- Deputy Side Lead – Watty Gaffney, Unite the Union – watty.gaffney@nhs.scot
- Health and Safety Forum
- Staff Side Lead – Andrew McCready, Unite the Union, Andrew.McCready@ggc.scot.nhs.uk (07479 658 758)
- Deputy Staff Side Lead – Teresa Will, GMB, teresa.will2@nhs.scot
- Inverclyde HSCP Staff Partnership Forum
- Staff Side Lead – Vacant
- Deputy Staff Side Lead – Vacant
- North Sector (Acute) Staff Partnership Forum
- Staff Side Lead – Elaine Quail, Unite the Union, Elaine Quail @ggc.scot.nhs.uk
- Deputy Staff Side Lead – Josh Cairns, Unison, jcairns@unisonglasgowclyde.com (Phone – 07557796275)
- Pharmacy Staff Partnership Forum
- Staff Side Lead – Josh Cairns, Unison, jcairns@unisonglasgowclyde.com
- Deputy Staff Side Lead – Simon Fraser, Unite the Union, Simon.Fraser@ggc.scot.nhs.uk
- Regional Staff Partnership Forum
- Staff Side Lead – Vacant – Watty Gaffney, Unite the Union – watty.gaffney@nhs.scot
- Deputy Staff Side Lead – Ciorstaidh Reichle, GMB, Ciorstaidh.Reichle@gmbactivist.org.uk (Phone – 0794211319)
- Renfrewshire HSCP Staff Partnership Forum
- Staff Side Lead – Annie Hair, Unite the Union, Annie.Hair@ggc.scot.nhs.uk
- Deputy Staff Side Lead – Robert Gibson, Unison, Robert.Gibson@ggc.scot.nhs.uk
- South Sector (Acute) Staff Partnership Forum
- Staff Side Lead – Frances Carmichael, Unison, fcarmichael@unisonglasgowclyde.com
- Deputy Staff Side Lead – Susan Walker, Unite the Union, Susan.Walker2@ggc.scot.nhs.uk (07724811532)
- West Dunbartonshire HSCP Staff Partnership Forum
- Staff Side Lead – Vacant
- Deputy Staff Side Lead – Andrew McCready, Unite the Union, Andrew.Mccready@ggc.scot.nhs.uk (07479 658 758)
- Women & Children’s Staff Partnership Forum
- Staff Side Lead – Watty Gaffney, Unite the Union – watty.gaffney@nhs.scot
- Deputy Staff Side Lead – Vacant
Employee Director’s Office
- Employee Director: Ann Cameron-Burns – Ann.Cameron2@ggc.scot.nhs.uk (Phone – 07557561923)
- Staff Partnership Lead: Elaine Quail – Elaine.Quail@ggc.scot.nhs.uk (Phone – 07490444464)
- Staff Partnership Lead: Ciorstaidh Reichle – kirsten.reichle@nhs.scot (Phone – 07949211319)
- APF Administrator: Kirstin.McKenzie@nhs.scot (Phone – 0141 201 4458)
Quick Links
Was this helpful?
This year the Chair, Prof John Brown CBE, presented two awards which recognise outstanding achievement, expertise, and dedication in patient care. In common with all the other awards, these celebrate our people’s collective efforts and the lasting impact they have had on the lives of the people of Greater Glasgow and Clyde.
Andrew Thomson
One of Andrew’s patients was going through a high risk pregnancy, when her husband sadly passed away after a two week battle with cancer. On hearing the news, Andrew called to offer his condolences and also talk about how he and his team could support the patient during this heart breaking time.
Andrew has an incredible way of communicating with patients and their families, with empathy and intuitiveness in abundance.
Unscheduled and Urgent Care Services
Due to unprecedented pressures, our Urgent and Unscheduled Care services have adapted to new and ever-changing situations which have been nothing short of remarkable. From the launch of the Flow Navigation Centre and Mental Health Assessment Units, to the ongoing dedication, commitment and professionalism of our EDs, IAUs, Community Pharmacies, MIUs, in-hours and Out of Hours GP Services, who have worked tirelessly with the support of diagnostic services.
At the start of the pandemic, it became clear that those who became very ill with Covid need a place where they could be seen and assessed safely and away from non-Covid patients.
Our Community Assessment Centres were created. This significant project required input from all of the eHealth teams to ensure the centres had all the necessary telephony and IT kit. They also needed to be set up very quickly.
eHealth teams responded to the needs of the service, working above and beyond to introduce new processes to book in Covid patients outwith hospital settings. The staff showed immense flexibility and changed their hours of work and their roles. The success of the CACs was due to the commitment, flexibility and team working across eHealth to support the Board in its response to the pandemic.
Was this helpful?
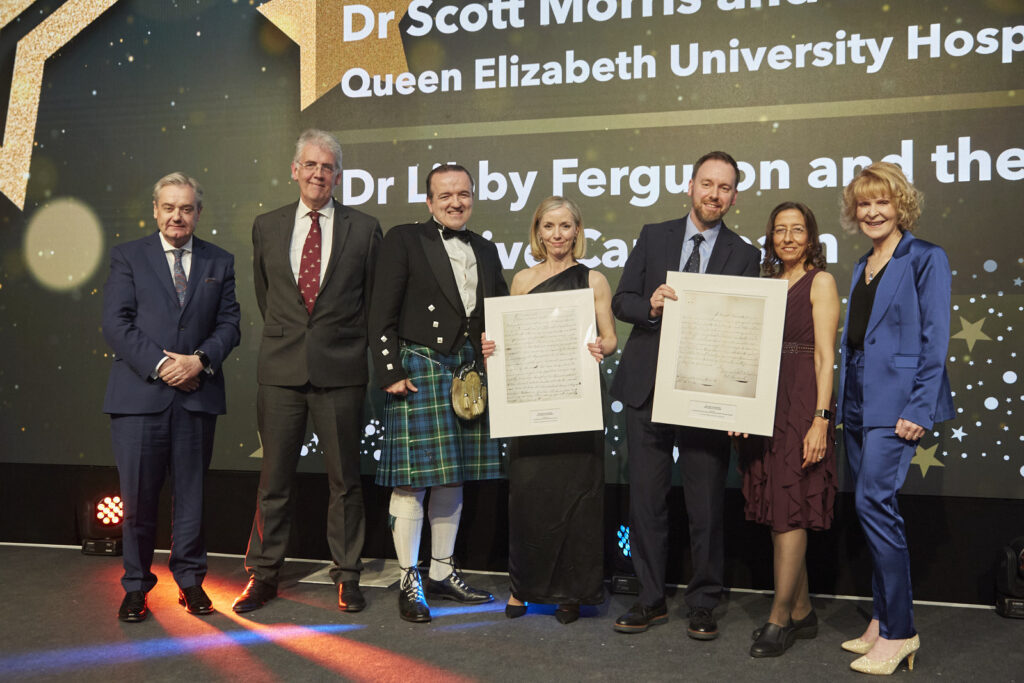
The William Cullen Prize for Excellence In Teaching and the William Cullen Prize for Service Innovation are awarded in collaboration with the Royal College of Physicians in Edinburgh.
William Cullen Prize for Innovation
Dr David Lockington is a Consultant Ophthalmologist based in Gartnavel General Hospital.
Dr Lockington identified the opportunity to transform unused rooms within the Tennent Institute of Ophthalmology library into a state of the art teaching suite for ophthalmology training. There are now three rooms which consist of an ophthalmic simulation area, a computer room for trainees and a seminar room.
The suite allowed simulated microsurgical skills to be developed and maintained during lockdowns, and is now used regularly by trainees and the wider multidisciplinary team. This development has been extremely well received by local trainees, and has addressed previously identified surgical training gaps.
Local ophthalmology training has been enhanced significantly, and to illustrate the impact, this initiative has since been replicated in other UK centres.
William Cullen Prize for Education – Joint Winners
Doctor Scott Morris is the Clinical Director for the Renal Unit, based in the Queen Elizabeth University Hospital, though which provides a full range of renal services to the West of Scotland.
This unit has for some time demonstrated a high standard of teaching and training, as evidenced by consistent and positive feedback from trainees. Trainees emerge as highly trained renal physicians, having been supported by a skilled group of established Consultants with a range of subspecialty interests.
The experience gained while attached to the unit is clearly valued by trainees, who highlight in particular the supervision they receive within the department, the supportive environment and the overall level of satisfaction working within a very strong team.
Dr Libby Ferguson and the Palliative care team based in the Marie Curie Hospice in Glasgow continue to provide an extremely high standard of clinical training which trainees recognise with positive responses to the Scottish trainee survey and National training survey.
There is a strong culture of educational governance identified within the centre. Trainees attached to the team there give very positive feedback in all areas, with Foundation trainees in particular highlighting the very supportive and educational environment provided by the team, and General Practice Specialty Trainees similarly appreciating the education and experience that is provided.
Was this helpful?

Staff Awards 2025
Every day our staff and volunteers go above and beyond to provide the best possible care and support to patients, relatives and staff. The Celebrating Success Awards held on 28th May 2025, are an opportunity for us to recognise that, and this year’s winners are fantastic examples of the hard work and incredible dedication all our staff display year round.
Every award winner and nominee should be immensely proud of themselves for the contribution they make to the delivery of healthcare in Scotland.
Find out about the winners and nominees from each award category below.
The winners were also announced live on the night on our social media channels (follow the #ggcawards hashtag).
View our photos from the 2025 Celebrating Success Awards event.

Previous Winners
You can read about the previous winners and nominees, watch videos, and view the photos from the awards event using the button below.
Nominate a Person, Team or Project
If you would like to nominate a person, team or project for an award please complete the relevant form below:
Was this helpful?
All NHS Greater Glasgow and Clyde employees can self-refer to the Occupational Health Service to access a wide range of confidential support services including counselling and psychological therapies.
The NHSGGC Staff Support and Wellbeing Hub can provide you with support in a range of areas:
- Money issues
- Weight management
- Mental health and wellbeing
- Peer support
- Emotional wellbeing
- Stop smoking
- Stress management
- Mindfulness
- Women’s health
Was this helpful?
The NHS Scotland Pension Scheme provides NHSGGC staff with a high-quality pension scheme that offers defined benefits at retirement and protection for your dependents based on your career average earnings.
The amount you pay towards your pension scheme depends on your ‘pensionable pay’ (which is your salary, wages, fees and any other regular payments but not any bonuses, expenses or overtime payments).
NHSGGC contributes 20.9% of your pensionable pay into the scheme on your behalf.
Key features of the NHS Scotland Pension Scheme include:
- Benefits accrued on a Career Average Revalued Earnings (CARE) basis.
- Normal pension age the same as the your State Pension Age.
- Pension accrual rate of 1/54th of pensionable earnings each year.
- Benefits for active members revalued each year using the Consumer Prices Index (CPI) plus 1.5%.
- Benefits for preserved members increased using the CPI each year.
- Valuable death benefits for your dependents.
- Option to take part of your pension and continue working.
- Enhanced pension for working longer than normal pension age.
- Option to purchase additional pension.
- Option to buy out the actuarial reduction if retiring from age 65 and before state pension age.
- Option to take up to 25% of pension pot as a tax-free lump sum.
Staff are welcome to opt-out of the NHS Scotland Pension Scheme at any time. Staff are also welcome to contribute to an alternative pension provider if this is preferable.
Was this helpful?
NHS Greater Glasgow and Clyde is a Living Wage employer and, as such, the lowest available salary of £23,240 translates into an hourly rate of £11.89 per hour, which is considerably above the Scottish Living Wage rate of £10.90 per hour.
- Agenda for Change is the NHS pay system for all staff directly employed by NHSGGC (with the exception of some very Senior Managers, Doctors, and Dentists). The current Agenda for Change salary scales can be viewed at the NHS Scotland Management Steering Group website.
- The salary scales for medical and dental professionals (including Consultants, Junior Doctors, the Scottish Public Dental Service, Specialty Doctors and Associate Specialists) can be viewed at the NHS Scotland Management Steering Group website.
- The salary scales for very senior managers (including executive directors and senior management) can be viewed on the NHS Scotland Publications library.
Was this helpful?
Our dedicated teams and individuals were nominated for the prestigious NHSGGC Excellence Awards by patients, visitors and staff. All of our staff have gone above and beyond in the past year and we asked to hear about your experience of outstanding care and for your nominations.
There are 7 categories in our Excellence Awards and the winners were announced at the Celebrating Success Event on 4th May 2023.
The winners were announced live on the night on our social media channels (follow the #ggcawards tag).
You can find out who the Gold Winners were, read about the Silver Winners who were shortlisted, and also view photos and videos in each of the categories below.
Congratulations to all our winners!
Better Care
This award recognises staff who provide and contribute towards incredible patient care improving everyday practices across NHSGGC.
Gold Winner – Dr Abigail Gunn
Dr Gunn has established the Medical Assessment Unit and Short Stay Unit at Inverclyde Royal Hospital, to facilitate rapid assessment of patients. These are aimed at reducing the number of hospital admissions and ED pressures, while ensuring patients continue to receive the highest standards of care possible.
This has all been facilitated by Dr Gunn while she continues her usual work place requirements, giving up her own time to ensure this was implemented. In addition, she is a focal point for the junior doctors and the advance nurse practitioners and also trainees rotating through the hospital, arranging inductions for these doctors and providing support, advice and supervision as required.

Silver Winners
Kay Anderson

Frailty Advanced Nurse Practitioner Kay Anderson has been nominated for a Better Care award after successfully setting up a primary care focussed frailty service covering every GP surgery in Inverclyde.
By offering polypharmacy reviews and anticipatory care planning, patients are receiving realistic medicine that suits their needs and prevents hospital admissions.
As well as this Kay has managed a Frailty MDT clinic comprising herself, a consultant geriatrician, physio and occupational therapist with links to other AHPs.
Kay’s service has been pivotal in treating patients in the community rather than putting further pressure on unscheduled care services in Inverclyde, with the service dealing effectively with the waiting list for geriatric falls and frailty reviews.

Andrew Thomson
One of Andrew’s patients was going through a high risk pregnancy when her husband sadly passed away after a two week battle with cancer. On hearing the news Andrew called to offer his condolences and also talk about how he and his team could support the patient during this heart breaking time.
Andrew has an incredible way of communicating with patients and their families, with empathy and intuitiveness in abundance.

Glasgow Royal Infirmary’s Nuclear Cardiology Team

Over the past two years, the Glasgow Royal Infirmary Nuclear Cardiology Team has launched the UK’s first routine service the assessment of Coronary Flow Reserve (CFR) via Single Photon Emission Computed Topography (SPECT) to reduce Major Adverse Cardiovascular Events (MACE).
SPECT usually involves patients having two 90 minute sessions of intensive imaging, but the team – in collaboration with centres of excellence in Italy and consultants in France – delivered a new technique which can require just one 45 minute treatment, reducing the radiation burden on patients by an average of 30 per cent.
This innovation is a UK-first, with the one day technique being adopted as routine last year.

Urgent and Unscheduled Care services
Due to unprecedented pressures our Urgent and Unscheduled Care services have adapted to new and ever-changing situations which have been nothing short of remarkable. From the launch of the Flow Navigation Centre and Mental Health Assessment Units to the ongoing dedication, commitment and professionalism of our EDs, IAUs, Community Pharmacies, MIUs, in-hours and Out of Hours GP Services, who have worked tirelessly with the support of diagnostic services.
At the start of the pandemic, it became clear that those who became very ill with Covid need a place where they could be seen and assessed safely and away from non-Covid patients.
Our Community Assessment Centres were created. This significant project required input from all of the eHealth teams to ensure the centres had all the necessary telephony and IT kit. They also needed to be set up very quickly.
eHealth teams responded to the needs of the service, working above and beyond to introduce new processes to book in Covid patients outwith hospital settings. The staff showed immense flexibility and changed their hours of work and their roles. The success of the CACs was due to the commitment, flexibility and team working across eHealth to support the Board in its response to the pandemic.
Better Health
This award commends staff who have implemented an initiative to improve the health and wellbeing of patients, the public and/or staff.
Gold Winner – Emergency Food Discharge Service
The Emergency Food Discharge Service was created by our Support and Information Services in partnership with the Aroma Café and GGC Foodbanks to help patients tackle the immediate cost of living challenge.
The team uses a referral process from clinicians to ensure no at risk patient or carer goes home hungry by providing a 2-day supply of food upon discharge. The intervention also enables conversations and support in relation to fuel for heating and money to be put in place prior to them going home.
The initiative has supported 1,000 patients as of January this year and is a fantastic example of how our acute, catering and our charitable organisations can work in partnership to meet the most basic, fundamental needs of our patients.

Silver Winners
Dr Alison MacBeth

Dr Alison MacBeth, a Speciality Doctor in Breast Surgery at Stobhill ACH Breast Clinic, has almost 10 years’ experience – but she undertook training to enhance her knowledge of menopause in her own time while maintaining her regular clinical commitments.
She is now recognised as a specialist menopause doctor, which has proved to be an invaluable addition to the service, with consultants from other hospitals now referring patients.
Her knowledge is reassuring to patients who attend her clinics, and by liaising with community GPs, she is able to advise on best practice on hormone replacement therapy, particularly in cases involving patients with a family history of breast cancer.

The Health For All Team

The Health For All Team set a target of improving the health of Unaccompanied Asylum Seeking Young People (UASYP) to ensure they are able to access appropriate health care that meets their needs.
This meant the team carrying out comprehensive health assessments for all UASYP under the age of 18 arriving in Greater Glasgow and Clyde, East Renfrewshire and East Dunbartonshire within 28 days of their referral to the service.
Many UASYP have known adversity or traumatic experiences on their journey to the UK, without any family support. The team sought to address many of the inequalities and challenges the young people faced and have taken on board the many learning opportunities this offered to inform future practice.
Better Value
This award is for staff who have increased efficiencies taking a new approach to work making better use of resources.
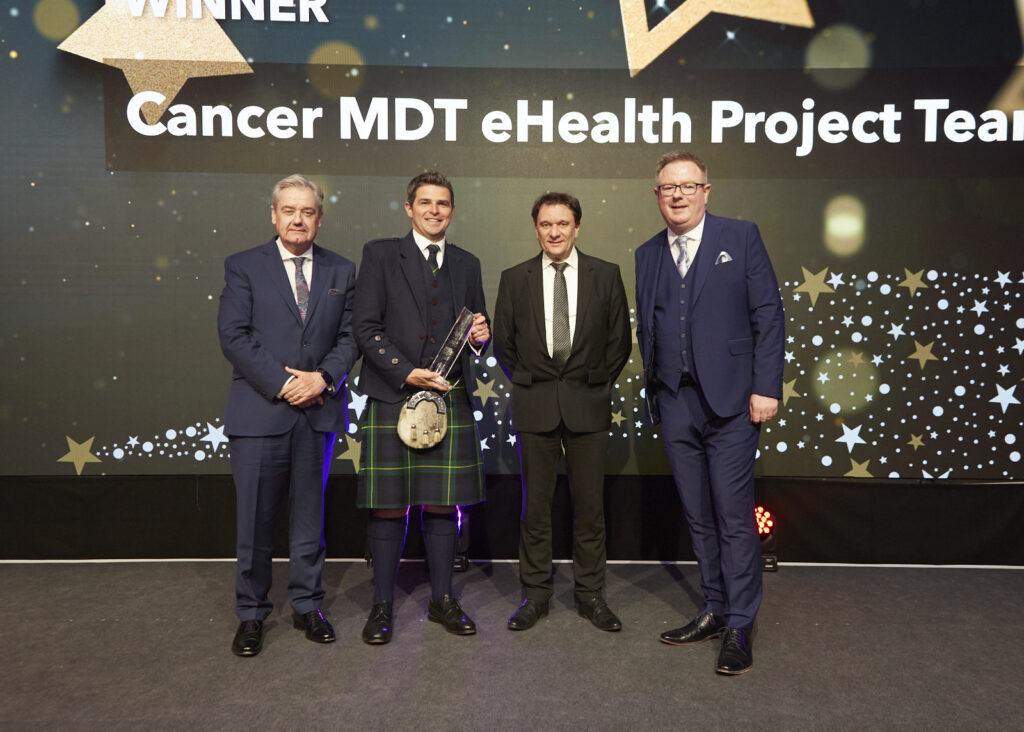
Gold Winner – Cancer MDT eHealth Project Team
The Cancer Multi-Disciplinary Team eHealth project team based at Glasgow Royal Infirmary have developed a digital solution to help streamline the MDT process, offering an ehealth solution that allows better cross board working and aligns MDT working to standardise referrals.
The project demonstrated its success through a live pilot for gynaecological cancers. In 2022, there were nearly 3000 patient episodes with the feedback from all users resoundingly positive.
This is now being adopted as the standard for cancer MDT’s across the West of Scotland with a matrix of regional eHealth departments supporting the development and support for the application as it is rolled out to each cancer type.

Silver Winners
Knowledge Services Team
The Knowledge Services Team at Gartnavel Hospital have been nominated for their contribution on the Adult Acute Care and Realistic Medicine apps as.
The team, made up of Michelle Kirkwood, Catriona Denoon, Fran Harkness and Amanda Wright, utilised their skills to organise mass amounts of clinical data into one, readily accessible format for both web and mobile either inside or out of a hospital setting.
Overcoming numerous obstacles, the team have worked to tight timescales and have been committed to delivering an influential and highly usable product.
The Realistic Medicine app was so highly thought of by the Scottish Government Realistic Medicine team, that it has been adopted as the framework and basis for a national Realistic medicine App for all NHS.

Paul Reid

Corporate Transport Manager Paul Reid worked through the Covid-19 pandemic to ensure transportation was adapted to accommodate vaccine deliveries in addition to existing regular services.
Since then, Paul has gone on to identify areas where efficiencies can be made with some services, such as the transport of renal dialysis patients, has been brought in-house.
This has meant Paul developing a network of colleagues in various disciplines to develop new ways of working together to improve service provision.
As a result, Paul is now being approached by clinical teams, seeking his advice on how transport services have be adapted to provide more cost effective ways of operating, in-line with the board’s ongoing financial improvement measures
Better Workplace
This award recognises the often unseen work of our staff who help make NHSGGC a better workplace, improving the culture and supporting colleagues.
Gold Winner – Elizabeth Thomson

Silver Winners
NHS Practice Education Team
The NHS Practice Education Team have created the Newly Qualified Practitioner (NQP) pathway for all newly qualified nurses, midwives and allied health professionals joining the organisation.
The pathway provides support to NQPs to the organisation throughout their first year in practice by offering a supportive culture and environment as they begin their careers.
By delivering sessions to final year students at university, the pathway informs NQPs of the various support mechanisms in place to allow them to highlight they are joining a supportive organisation which has been shown to lead to improved patient care outcomes and retention of staff.
The team regularly evaluate their input for the supports in place to ensure if any changes are required with the feedback being overwhelmingly positive since the outset.

Rachel McGowan

Rachel is a Witness Support Manager based at West Glasgow Ach and has been influential in providing practical and emotional support and guidance on court and legal process for staff who are required to participate in court or legal proceedings.
Initially, Rachel was volunteering in the role before securing a permanent position to support staff across acute, corporate and partnership settings.
In recent months, the demand on Rachel’s services has increased substantially, yet she has continued to go over and above to provide support to all staff who have contacted her.
Although anonymous, the feedback that has been provided for Rachel has been unequivocally positive as she continues to deliver a unique service.

Liz Thomson
As part of the Complex Needs Service, Liz went beyond her role as a Health Care Support Worker, and provided extra support to fellow staff members through “Lizzie’s Lunch Club”.
Liz made sure members of the mental health team were able to get a healthy lunch despite their busy daily schedules. She would use her own lunch break to make sure staff were able to eat properly, even making packed lunches for staff on outreach visits as well as care packages for patients, ensuring they had adequate items at their time of need.
Staff said that Liz’s initiative helped them going through their often very busy days and the fact that she is so giving to colleagues and patients was worthy of special recognition.
Global Citizenship
This award recognises staff who have travelled overseas to provide healthcare and/or education in developing countries or countries in crisis.
Gold Winner – Katie Earle-Payne
Providing healthcare for 1,500 Ukrainian refugees aboard the MV Ambition cruise ship posed a number of challenges – but Senior Pharmacist Katie Earle-Payne’s unique skill set allowed her to help offer outstanding patient care.
Katie speaks, reads and writes Ukrainian and was able to work as a prescribing pharmacist on-board MV Ambition without needing translation services.
She developed pathways for GP support for refugees as well as other specialities and was able to keep refugees accurately informed about treatment as some medicines prescribed in Ukraine are not available in the UK and alternatives had to be identified.
With just two weeks’ notice, Katie worked three days per week on board MV, providing in-person advice and consultations and acting as a link between patients and other services.

Silver Winners
Infant Feeding Educational Delegation to Lahore Children’s Hospital

The Royal Hospital for Children in Glasgow (RHC) has been twinned with the Children’s Hospital and University of Child Health (CHICH) – a government hospital in Lahore, Pakistan since 2001. CHICH is now the largest children’s unit in Pakistan with 1100 beds and deals daily with thousands of outpatients on very limited resources.
In recent years, the Infant feeding educational delegation has worked hard to help the hospital tackle challenges associated with breastfeeding currently facing mothers and babies. They delivered a 4-day infant feeding programme which was attended by more than 60 staff locally, coupled with a one-day programme of lectures. This is helping create breastfeeding trainers and champions locally and improving outcomes for infants in Lahore.
This type of global collaboration where each member of a partnership benefits is the essence of global citizenship.

Asylum Health Bridging Team

MV Ambition cruise ship was berthed in Glasgow, accommodating Ukrainian 1,500 refugees since September last year, until they can find longer term homes across Scotland.
Stewart is the Asylum Bridging Team (ABT) Lead and worked extremely hard, alongside his colleagues, to ensure there was a streamlined system and processes in place supporting Ukrainian refugees to access health care. The ABT were on board the ship providing those residing there initial health assessments, translated information documentation, signposting, and supporting the GP registration process. Stewart was supported by Ukrainian Senior Pharmacist Katie Earle-Payne, who provided medical translations and eased any worries patients had.
As the refugees settle into more permanent accommodation, across NHS Greater Glasgow and Clyde, Stewart and his team continue to support these patients and their GP colleagues.
Nursing
This award recognises nurse(s) who demonstrate the best qualities of patient care and the ethos of nursing.
Gold Winner – Charlotte Picken
Senior staff nurse Charlotte Picken based at the Royal Hospital for Children was the first nurse to identify a need for nurse prescribing in theatre recovery and drive the project through to completion.
After carrying out an audit, Charlotte highlighted the prolonged suffering of children in pain while waiting for additional analgesia to be prescribed by anaesthetic staff. This had a knock on effect by interrupting routine theatre services as anaesthetists were required to attend recovery to prescribe.
As a result, this has reduced suffering of post-operative pain as waiting times for analgesia have significantly improved with additional feedback from nursing and medical colleagues to support this.

Silver Winners
Marie Cairnie
Marie has been a Nursing Assistant in Dykebar Hospital for 48 years. She has been based in Continuing care for a great many years, working with elderly male patients with significant cognitive decline.
Marie is approaching 75 years of age and could have retired years ago, but she has chosen to continue working and serving our most vulnerable patient group.
She is committed to maintaining the dignity of her patients, but it is her energy and positivity that singles her out among her colleagues. She brings laughter and joy to her patients and workmates alike.
In addition, Marie knows her experience is invaluable to younger colleagues and she is happy to pass on her knowledge to others. She is very much an “old school nurse” in every sense of those words.

Pamela Charles

Pamela Charles is a specialist mental health nurse who provides essential support to young people in their homes, completing mental health assessments and ensuring they get the treatment they need.
One day in between visits, Pamela spotted a male on the wrong side of the safety railings on a bridge and immediately she kicked into action.
After alerting emergency services, Pamela used her suicide first-aid training, supporting the individual and eventually talking him back to the safety of the bridge. On that day, Pamela’s quick thinking and compassionate approach helped avoid a fatal accident.
Her response embodies nursing practice. She even continued to her next appointment to ensure the young person she was seeing received the support and care they needed. Pamela herself saw her actions as ‘all in a day’s work’ which further evidences the humility she applies to the way she approaches her job.

Recovery Staff Theatres
The team works hard to ensure every child is re-united with their parents or carers as soon as possible after surgery. Seeing their child go for surgery can often be a hugely anxious and stressful time for families, parents and carers and for a child to wake up and see familiar faces can be distressing.
The staff within recovery understand the difference it makes having parents and carers involved in the process and the benefits of them being re-united with their child as soon as possible. An innovative pager system has been implemented, which allows the team to stay in touch with families and eliminates mobile phone signal issues. This system means the recovery team can meet with parents and carers as their child goes into theatre, introducing themselves and giving any information they might need, putting them at ease.
Volunteer
Recognising people who go the extra mile contributing tirelessly and providing outstanding help and support for the benefit of others.
Gold Winner – The Rainbow Garden, Larkfield Unit
After seeing a patch of ground at the Larkfield Unit at Inverclyde Royal Hospital, Sandra Forbes set about transforming it into a colourful, tranquil green garden enjoyed by patients, visitors and community groups. With the help of NHS Greater Glasgow and Clyde staff, volunteers and donations from local people and businesses.
While this was the brainchild of Sandra, social worker Fiona McInnes loved the garden and donated some money which helped to transform the courtyard area of the Larkfield Unit, before she passed away suddenly. Fiona is still a key part of the garden and is remembered each day in the garden through a special memorial.

Silver Winners
Margaret Gunduz
Among all specialties across NHSGGC, our volunteers make among the most significant differences to patients, staff and members of the public.
Margaret Gunduz is a Discharge Lounge Volunteers at the Royal Alexandra Hospital and, without her, patients waiting to leave our care would have a far less positive experience.
The main role of our Discharge Lounge volunteers is to provide companionship and stimulation for patients, offering a distraction whilst they wait to be discharged from their hospital stay.
Margaret is a very welcome extra pair of hands in the lounge, and she has become one of the best-known faces at the RAH. Everybody knows her, and her caring, proactive approach to our patients singles her out as a particularly special member of the RAH team.

Naloxone Peer Champions
The Peer Naloxone Programme was introduced to combat the drug death crisis in Scotland.
It offers training to anyone who might come into contact with someone experiencing an overdose to administer Naloxone which can reverse overdoses and save lives.
Our Naloxone Peer Champions are volunteers living in prisons who are able to provide crucial training on overdose awareness and Naloxone to prisoners and those leaving prison. This service is unique and our champions are helping make the communities that people return to safer and contribute to the reduction of drug deaths in Scotland.
Since November 2021, the champions have trained more than 745 people. There are now 12 champions working in HMP Low Moss, Barlinnie and Greenock and together they are helping equip more people than ever before to save lives.