Mood changes are a necessary part of human functioning. It’s natural to feel anxious, worried, sad or low sometimes. But when mood changes become severe, persistent and interfere with normal life, we need to take notice.
The persistent low mood of depression is deeper, longer and more unpleasant than the short periods of unhappiness we all have from time to time. Similarly, persistent anxiety is more than just feeling worried. Many people experience symptoms of depression and anxiety at the same time. Significant depression or anxiety affects more than one in ten people during their life.
More Information
Depression – Introduction
Depression is a very personal experience. Symptoms can vary from person to person but usually include changes to your:
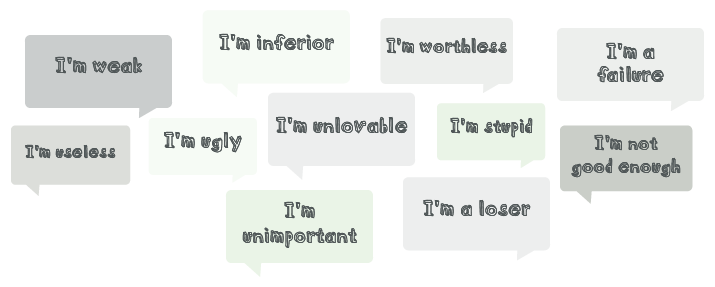
- Thoughts (for example feeling worthless or to blame, hopeless and incapable)
- Mood (feeling persistently down, anxious, or numb)
- Behaviour (for example losing interest or pleasure in previously enjoyed activities).
You may also notice physical changes such as loss of appetite, tiredness, or aches and pains.
Depression can come on gradually so it can be difficult to notice something is wrong.
Many people continue to cope with their symptoms without realising they are ill. It can take a friend or family member to suggest that something might be wrong.
The most common symptoms of depression are:
- Little interest or pleasure in life
- Feeling down, hopeless, numb or empty
- Sleep disturbances. Difficulty falling or staying asleep. Sleeping too much
- Tiredness and lack of energy
- Appetite disturbances. Not eating enough, or overeating
- Feeling bad about yourself. Feeling like a failure, believing that you have let other people down
- Difficulty concentrating on things like reading or watching television
- Moving or speaking much more slowly. Or becoming fidgety or restless
- Thinking about death and dying. Thinking about harming yourself. Wondering if you would be better off dead.
People may find themselves worrying excessively over the smallest things, blaming themselves for everything that goes wrong, and feeling irritated by those around them.
Depression has been described as a “heavyweight” “a state where nothing tastes, smells or feels right” or “being in a world without colour or laughter”.
Depression can cause bleak and distressing thoughts, including suicidal thinking and planning. With support and treatment, the negative feelings often pass.
If you are unsure whether what you are experiencing is depression, the following questionnaire might help you decide whether you should get help PHQ9.
Anxiety – Introduction
Anxiety is a feeling of unease, worry, or fear. Everyone feels anxious sometimes, but for others, it can be an ongoing problem. A bit of anxiety can be helpful; for example, anxiety before an exam can keep you alert and improve performance. Too much anxiety, however, affects focus and concentration.
Some of the most common symptoms of anxiety are:
- Feeling uneasy a lot of the time
- Having difficulty sleeping, feeling tired
- Poor concentration
- Being irritable
- Being extra alert
- Feeling on edge, not being able to relax
- Needing lots of reassurance from others
- Tearfulness
When you’re anxious or stressed, your body releases stress hormones, such as adrenaline and cortisol. These cause the physical symptoms of anxiety which include:
- A pounding heartbeat
- Breathing faster
- Palpitations (an irregular heartbeat)
- Feeling sick
- Chest pains
- Headaches
- Sweating
- Loss of appetite
- Feeling faint
- Needing the toilet
- “Butterflies” in your stomach.
Anxiety symptoms can happen occasionally or regularly. They may start suddenly or come on gradually. They can be a nuisance or extremely disabling. Specific anxiety disorders include:
- Panic disorder (when you have panic attacks)
- Post-traumatic stress disorder
- Generalised anxiety disorder
- Social anxiety
- Specific phobias
What helps
Regular exercise can be very effective in lifting mood and increasing energy levels. Exercise can help improve appetite and sleep. The research behind this shows that physical activity stimulates chemicals in the brain called endorphins, which can help you to feel better. Inactivity can cause a vicious circle: the less you do, the less you want to do. It is also important to eat well. If you aren’t eating regular healthy meals, your body won’t have enough energy, leaving you lethargic and slow.
Although you may not feel like it, keeping in touch with people can help you feel a bit more grounded and sometimes put things in perspective. Try a short phone call to a close friend or relative, or an email or text.
Try to avoid too much stress, including work-related stress. If you’re employed, you may be able to work shorter hours or work in a more flexible way, particularly if job pressures seem to trigger your symptoms.
Be kind to yourself! Depression and anxiety can make you feel inadequate or worthless. It’s hard to do nice things for yourself when you feel like that. As soon as you feel able, do something enjoyable for yourself or someone else.
Depression and anxiety can make everyday tasks overwhelming. It can help to break things down into smaller, more manageable steps. Set yourself a goal each day, starting with something small and working up to bigger tasks that you may have been putting off.
When you feel ready, you may find it helpful to do something to help other people, as this may help overcome feelings of isolation, take your mind off your own problems and make you feel better about yourself. The Scottish Recovery Network encourages people to share their personal journeys to recovery. Reading and sharing stories of hope, optimism, and strength can help balance the negativity of depression and can help an individual feel more in control of their own life again.
Learning how to relax and be mindful can also be helpful in your recovery.
Overcoming depression and anxiety can take time but there is treatment available. Most people recover. Understanding yourself helps – learning to recognise your own ‘warning signs’ of how you react under stress, or when things become difficult, is an important part of staying well in the future.
Find out more
There are times in our lives when many of us will experience feelings of low mood and anxiety.
There is more information about the symptoms on MyApp: My Mental Health and NHS Inform.
The Scottish Association for Mental Health offer community-based services for people with mental health problems and has a role in policy development and campaigning on mental health issues.
Helping someone else
There is helpful information on the NHS Inform webpage on supporting someone with Depression if you’re worried about someone you care about or care for who is depressed.
If you’re caring for someone with a mental health difficulty these organisations can offer support:
Self Help Resources
Self-help guides are also available on MyApp: My Mental Health, NHS Inform and Get Self Help
Looking after someone with…Depression & Anxiety
Depression and anxiety cause feelings of sadness, guilt, despair and hopelessness. Self- esteem and confidence can be badly shaken.
People with depression or anxiety may avoid their friends and relatives rather than ask for help or support. This is often when they need your help and support most.
How do you help someone who may not want your help, or feel they deserve help? You can help by just being there. Showing a real interest in them, not just their problems. Be prepared to listen, and to spend time with them. This can help counter the unpleasant, negative thoughts they will have about themselves.
Someone who is depressed may need a lot of encouragement to get help. You could find out about local support groups, relaxation classes, or self-help literature. You could offer to go with them to a group or doctor’s appointment.
Sometimes it can feel that the person you know and love has changed so much, you find it hard to recognise them. If you have serious concerns about their well-being or think they may be suicidal urgent help is needed. You can call their GP or go to accident and emergency.
Supporting a friend or relative who is depressed or anxious can be an opportunity to build a closer and more satisfying relationship. However, it can be hard work and frustrating. You might feel helpless or annoyed if the person won’t accept your help. Unless you pay attention to your own needs, it can make you feel unwell too. Finding a support group and talking to others in a similar situation might help.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site.
BSL – Depression & Anxiety
NHSGG&C BSL A-Z: Mental Health – Depression
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. it affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and sometimes you may feel as if life isn’t worth living.
NHSGG&C BSL A-Z: Mental Health – Anxiety
Anxiety is a feeling that we can all get but sometimes it can become excessive and stop you from doing the things you want to. These feelings can become a problem when they cause distress or make us feel uncomfortable. There are various types of anxiety disorders depending on how often they occur or if they are triggered by certain things. Examples might be when the feelings of anxiety can occur all the time for no apparent reason with lots of worrying thoughts and physical symptoms such as a racing heart, feeling breathless, knot in your stomach, increased sweating. This is called Generalised Anxiety. Sometimes these symptoms can occur without warning for short periods of time for no apparent reason. These are called Panic attacks. Sometimes the feelings of aniety can be brought on by specific things such as a fear of heights or crowded places or spiders etc. These are described as Phobias.
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde.