In the same way that we all have physical health we also all have mental health. In much the same way as we experience ups and downs in our physical health, we can also face ups and downs in our mental health. We are all vulnerable to experience times in our life when we struggle to maintain a sense of balance and well-being which causes us to experience mental health issues. This can also be true in pregnancy where all women experience perinatal mental health – both good and not so good.
When it’s not so good it can also be known as ‘perinatal mental health problems’, ‘perinatal mental illness’ or ‘depression and anxiety in the perinatal period’.
It is important to know that there is always someone you can turn to for help and support and it’s ok to tell your midwife/GP/health visitor if you’re struggling.
Pregnancy can be both an exciting and worrying time for parents-to-be. Pregnant women experience a range of physical and emotional changes, all of which may trigger low mood or anxiety. It’s completely normal to feel excited about your pregnancy but also have moments of feeling worried or scared. Pregnancy – and having a baby – is life-changing so it’s natural to experience a range of feelings including low mood or anxiety. Try making some small changes in your life, such as taking some time out for yourself to relax, talking about your problems or getting more rest or sleep, can usually improve your mood. The good news is that low mood will tend to lift after a few days or weeks.
Low mood and anxiety during or after pregnancy doesn’t necessarily mean that you have perinatal depression. However, if you feel that your condition is worsening and suspect that it may be progressing to depression, it is important to speak to your GP or Midwife. Signs of this happening include more frequent bouts of low mood, finding it difficult to improve your mood and the inability to feel happy.
Up to one in five women and one in ten men are affected by mental health problems during pregnancy and the first year after birth. Unfortunately, only 50% of these are diagnosed. Without appropriate treatment, the negative impact of mental health problems during the perinatal period is enormous and can have long-lasting consequences on not only women, but their partners and children too. However, this is not inevitable. When problems are diagnosed early and treatment offered promptly, these effects can be lessened.
Sometimes there is an obvious reason for low mood and anxiety during or after pregnancy, but not always. You may feel distressed, or guilty for feeling like this, as you expected to be happy about having a baby. However this can happen to anyone and it is not your fault.
It’s never too late to seek help. Even if you have low mood or anxiety or have been depressed for a while, you can get better. The help you need depends on how severe your illness is. Mild symptoms can be helped by increased support from family and friends.
If you are more unwell, you will need help from your GP and health visitor. If your Low mood or anxiety is prolonged and severe, you may need care and treatment from a mental health service.
Myths about Perinatal mental health
Perinatal depression is often misunderstood and there are many myths surrounding it. These include:
- Perinatal depression is less severe than other types of depression. In fact, it’s as serious as other types of depression.
- Perinatal depression is entirely caused by hormonal changes. It’s actually caused by many different factors.
- Perinatal depression will soon pass. Unlike the “baby blues”, perinatal depression can persist for months if left untreated. In a minority of cases, it can become a long-term problem.
- Perinatal depression only affects women. Research has actually found that up to 1 in 25 new fathers become depressed after having a baby.
When does Perinatal mental health occur?
The timing varies. About a third of women with Perinatal mental health have symptoms which started in pregnancy and continue after birth. Post Natal Depression often starts within one or two months of giving birth.
Acknowledgement: Royal College of General Practitioners Perinatal Mental Health Toolkit
More Information
What is Perinatal Mental Health?
Around 1 in 10 women will experience postnatal depression after having a baby. However depression and anxiety are equally as common during pregnancy. Most women recover with help from their GP, health visitor and midwife, and with support from family and friends. However severe depression requires additional help from mental health services.
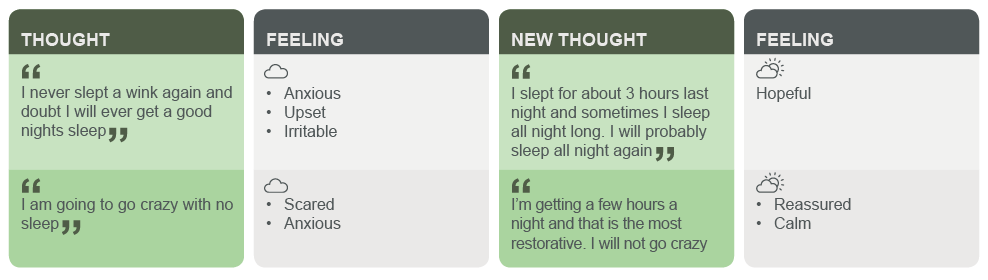
The symptoms of postnatal depression are similar to those in depression at other times. These include low mood, sleep and appetite problems, poor motivation and pessimistic or negative thinking.
Two in 1000 women will experience postpartum psychosis. The symptoms of this illness can come on quite rapidly, often within the first few days or weeks after delivery, and can include high mood (mania), depression, confusion, hallucinations (odd experiences) and delusions (unusual beliefs). Admission to a Mother & Baby Unit (MBU) is advised for most women, accompanied by their baby. Women usually make a full recovery but treatment is urgently necessary if symptoms of postpartum psychosis develop.
What helps
The following advice on how it feels to be unwell and what was, and what was not, helpful, is from a member of the Maternal Mental Health Scotland (MMHS) change agents, people with lived experience of Post Natal Depression (PND). This member had PND after having their daughter two years previously. They were also diagnosed with anxiety & depression which was noted as potentially sparked from suffering from PND.
“What does it feel like to be unwell – uncontrollable, lonely, crazy, low, tired, lack of energy. The only way I could describe it, is to say how low and crazy I felt. I felt when everything went right and my baby was “settled” I had a great day but as soon as we had an unsettled day, the smallest thing would set me off into a downer of a mood that I felt I couldn’t shift. It felt like someone was controlling my mind and body and I was in a deep hole I couldn’t get out of. Horrendous and sad feeling. I had so much support and amazing family around me yet I pushed them all away and wanted no one.
“What was helpful ” – speaking to people I wasn’t close to. Finding a really helpful & understanding doctor who would take the time out and listen to my true feelings and understand the severity. Speaking to other mums who were going through the same & also advising my family on my feelings.
“What was not helpful ” – the first doctor I got tried to put it down to baby blues when I KNEW there was something wrong. I was told that having PND, it isn’t that common you would pick the problem up by yourself. I was in tears and broke down explaining that I isn’t want my baby anymore, I wanted to get in my car and drive as far away as possible and never come back, I wanted a different life.”
Living with…Peri-Natal Depression
For patients
Mental health in pregnancy and the postnatal period
- SIGN Guidelines: Patient Information
- RCPsych: Mental health information on perinatal disorders
- Action on Postpartum Psychosis: Insider Guides
For professionals
Resources for healthcare staff
- Maternal Mental Health Scotland
- NSPCC Scotland & Maternal Mental Health Scotland: Getting It Right for Mothers and Babies-Closing the gaps in community perinatal mental health services
- LSE & Maternal Mental Health Alliance: Costs of perinatal mental health problems
- Everyone’s Business: Maternal Mental Health
Looking after someone with…Perinatal Depression
Involvement of partners and significant others
We will ask for your consent before sharing any information with friends, family members and carers.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Carers support
A carer is someone who looks after a partner, relative or friend who cannot manage without help because of illness, frailty or disability. They may or may not live together.
If you would benefit from support in your caring role, local carers services can help. They can provide you with help and support regarding a number of issues including access to respite, short breaks, information and advice on a wide range of topics, emotional support and access to carers support groups. To find information about your local carers service anywhere in Scotland please contact
The Carers Information Line
Telephone: 0141 353 6504
Email: info@glasgowcarersinformation.org.uk
Support for young people
- YoungMinds is a leading UK charity committed to improving the emotional well being and mental health of children and young people.
- Baby Buddy, urgent access to mental health services – available 24 hours per day
- Working hours: Your GP can refer you to the local Community Mental Health Team (CMHT) or Crisis Intervention Team
- Out of hours: Call NHS 24 on 111
- Bluebell PND service Glasgow – 0141 221 1535
- Crossreach
- Home Start Glasgow North – 0141 9482289, email info@homestartglasgownorth.org.uk
- NHSGGC Perinatal Mental Health Service
Your Midwife, GP and Health Visitor can offer support and advice.
BSL – Peri-Natal Depression
Postnatal depression (PND) affects around 10% of mothers. This is much more serious than the period post birth known as ‘baby blues’ which usually lasts between one to three days. PND can develop slowly and may not be noticeable until several weeks after the baby’s birth, or may continue on from the baby blues period. The symptoms of postnatal depression are similar to those in depression at other times. These include low mood, sleep and appetite problems, poor motivation and pessimistic or negative thinking. It can have a significant impact on the health and wellbeing of the mother and the child.
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde.
BSL – Postpartum Psychosis
NHSGG&C BSL A-Z: Mental Health – Post-Partum Psychosis
It is a severe episode of mental illness which begins suddenly in the days or weeks after having a baby. Symptoms vary and can change rapidly. They can include high mood (mania), depression, confusion, unusual experiences and strange thoughts. Postpartum psychosis is a psychiatric emergency. You should seek help as quickly as possible.
Postpartum psychosis can happen to any woman. It often occurs ‘out of the blue’ to women who have not been ill before. It can be a frightening experience for women, their partners, friends and family. Women usually recover fully after an episode of postpartum psychosis.
It is much less common than Baby Blues or Postnatal Depression. It occurs in about 1 in every 1000 women (0.1%) who have a baby
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde