Vaccinations
Why immunise?
The development of effective vaccines has led to a huge decrease in childhood deaths. The World Health Organization (WHO) states: ‘The 2 public health interventions that have had the greatest impact on the world’s health are clean water and vaccines.’
Benefits for you
As children develop they’re exposed to many risks, one of these risks being infections. Most of these will cause mild illnesses. However, despite great medical advances, infection can still cause severe illness, disability and, at times, death.
Before vaccines were available, many children in the UK died from diseases such as whooping cough, measles and polio. Despite successful immunisation programmes, the diseases that vaccines protect against do still exist.
The benefit of immunisation is that your child has the best possible protection against dangerous diseases. This can give you peace of mind.
Changes to childhood vaccinations – from 1st of July 2025
What parents and caregivers need to know
Experts regularly review the vaccination programme to make sure it gives children the best protection. New research and changes in vaccine supply mean the vaccination schedule in Scotland has changed.
If your baby was born on or before the 30th of June 2024, they will already be mid-vaccine schedule and will remain on that schedule until it is complete. There is no action required from you and your baby will be invited for these vaccinations when the time approaches.
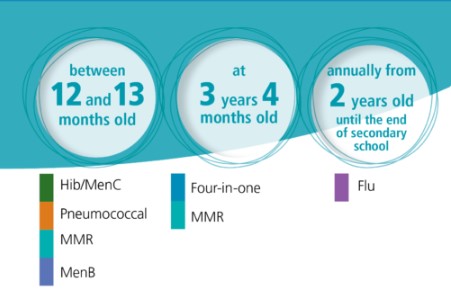
If your baby was born on or before the 30th of June 2024, they will continue to follow this schedule.
- 12-13 months – HibMenC, Pneumococcal, MMR, MenB
- 3 years 4 months – Four-in-one, MMR
- From 2 years old – Flu
The following changes came into place on the 1st of July 2025.
- 8 weeks – Six-in-one, Rotavirus, MenB
- 12 weeks – Six-in-one, Rotavirus, MenB
- 16 weeks – Six-in-one, Pneumococcal
- 12-13 months – MenB, Pneumococcal, MMR
- 18 months – Six-in-one, MMR
- 3 years 4 months – Four-in-one

If your child turned one year of age on or after 1 July 2025 (DOB on or after 1 July 2024), they will pick up on this schedule from here:
- 12-13 months – MenB, Pneumococcal, MMR
- 18 months – Six-in-one, MMR
- 3 years 4 months – Four-in-one
What’s changing?
Some vaccines will now be given at different times, and a new appointment will be added when your child is 18 months old.
Who decides this?
The changes are based on advice from the Joint Committee on Vaccination and Immunisation (JCVI) – a group of independent experts who guide the UK and Scottish vaccination programmes.
What happens next?
There is no action required from you. You’ll be given clear information when it’s time for your child’s next vaccinations.
Why is this important?
Vaccines are the best way to protect your child from serious illnesses. These updates help make sure the programme stays safe, effective, and up to date.
Changes to the routine childhood vaccination schedule
Changes to the routine childhood vaccination schedule from 1 July 2025 and 1 January 2026
Changes to be implemented
Phase 1 (from 1 July 2025)
MenB vaccination will now be offered from 12 weeks (previously 16 weeks).
- Following a recent clinical study and a review of the epidemiology, the JCVI has advised bringing forward the second dose of the MenB vaccine to provide earlier protection against this serious and sometimes fatal infection.
- Meningococcal serogroup B is responsible for the majority of UK invasive meningococcal disease (IMD) cases. Since the introduction of the routine MenB vaccination programme, peak age of infection has shifted from 5 to 6 months to 1 to 3 months of age. A substantial proportion of cases were occurring before infants gained protection from their second dose of vaccine given at 16 weeks. The change in epidemiology of IMD means it would be beneficial to move the second dose of MenB vaccine to 12 weeks of age to provide earlier protection.
- Although previously an 8-week interval between doses of MenB vaccine was recommended, evidence from a recent study showed a good response was made when the 2 doses were given 4 weeks apart.
Pneumococcal vaccination will now be offered from 16 weeks (previously 12 weeks).
- To avoid increasing the number of injections at the 12-week appointment, the first dose of the pneumococcal vaccine will be moved to the 16-week appointment.
- The change is unlikely to be clinically significant.
The Hib/MenC vaccine (Menitorix) will no longer be available.
- The manufacturer has ceased production of Menitorix vaccine. There is no other Hib/MenC vaccine available on the UK market.
- Children turning one year of age on or after 1 July 2025 (date of birth on or after 1 July 2024) will not have received the combined Hib-MenC vaccine (Menitorix) when they are invited for their 12-month vaccination appointment (they should still receive the other vaccines due at that age). These children should be offered a new 18-month routine vaccination appointment (starting from 1 January 2026) for a 4th dose of the 6-in-1 vaccine (DTaP/IPV/Hib/HepB (hexavalent)) vaccine, given alongside the second dose of MMR.
- The JCVI has agreed that protection against MenC is no longer required in this age group due to the high uptake of vaccination in the secondary school programme. Sustaining high uptake of the MenACWY vaccine, currently offered to S3 pupils, is important to maintain indirect protection.
Phase 2 (from 1 January 2026)
From January 2026, the MMRV vaccine will be offered as part of the routine childhood immunisation schedule. It replaces the MMR vaccine.
The MMRV vaccine protects against measles, mumps, rubella, and varicella (chickenpox). These are serious diseases that can be life-threatening.
Measles is a very infectious virus. It spreads easily though the air when people with the virus cough or sneeze. It can cause serious health complications, like pneumonia and encephalitis. In very serious cases, measles can be life-threatening.
Mumps is caused by a virus. It can cause permanent deafness, viral meningitis, and encephalitis. Mumps spreads through the air when people with the virus cough or sneeze, and is very infectious.
Rubella is caused by a virus. If caught in pregnancy, it can cause a miscarriage or affect the unborn baby. It can cause a condition called congenital rubella syndrome (CRS), which damages a baby’s sight, hearing, heart and brain. Rubella is spread through the air when people with the virus cough or sneeze, and is very infectious.
Varicella (chickenpox) is a highly infectious disease caused by a virus. Varicella is spread through direct contact with someone who is infected.
Read more about why your child should get the MMRV vaccine
Who can get the MMRV vaccine
The MMRV vaccine is offered to children as part of the routine childhood vaccination programme. When your child will be offered the vaccine depends on when they were born.
If your child was born on or after 1 January 2025
If your child was born on or after 1 January 2025, they’ll be offered 1 dose of the MMRV vaccine at both:
- 12 to 13 months
- 18 months
If your child was born between 1 July 2024 and 31 December 2024
If your child was born between 1 July 2024 and 31 December 2024, they’ll be offered a dose of the MMRV vaccine at:
- 18 months
- 3 years 4 months
If your child was born before 30 June 2024
If your child was born before 30 June 2024, they’ll be offered a dose of the MMRV vaccine at 3 years 4 months.
Introduction of a new 18-month appointment where the additional 6-in-1 (4th dose) vaccine will be offered.
- To replace the Hib dose, an additional dose of the 6-in-1 ((DTaP/IPV/Hib/HepB (hexavalent)) vaccine will be offered at a new routine appointment at 18 months.
- Children turning one year of age on or after 1 July 2025 (date of birth on or after 1 July 2024) will not have received the combined Hib-MenC vaccine (Menitorix) when they are invited for their 12-month vaccination appointment (they should still have received the other vaccines due at that age). These children should be offered a new 18-month routine vaccination appointment (starting from 1 January 2026) for a 4th dose of the 6-in-1 vaccine (DTaP/IPV/Hib/HepB (hexavalent)) vaccine, given alongside the second dose of MMR.
The second dose of MMRV will be brought forward from the 3-year 4-month appointment to the new 18-month appointment.
- The second MMRV dose is being moved forward in the schedule to provide earlier protection and, hopefully, help to improve uptake. Research showed moving the second dose of MMR forward in London led to higher uptake.
Queries about scheduling
My children are different ages, will they be on different schedules?
Yes your children might be on different schedules as the schedule children follow is dependent on their date of birth. When changes to vaccination programmes happen, they must be rolled out on a phased basis to ensure NHS immunisation teams are able to deliver the vaccines effectively alongside other programmes. Changes to programmes are based on the advice of the Joint Committee on Vaccination and Immunisation (JCVI). These decisions are based on several factors, including the risk of the disease and the effectiveness of the vaccine.
If I delay my child’s vaccines, will they change schedules?
The schedule your child follows is dependent on their date of birth not when they attend for vaccination. Do not delay getting your child vaccinated – they will not change schedules. It’s important that vaccines are given on time to make sure your child has the best protection possible. Delaying or missing vaccine doses can put your child at risk of serious diseases and getting vaccines when they are due is the best way to protect your child.
Pre-School Children
The 6-in-1 Vaccine
Overview
The 6-in-1 vaccine, also commonly known as the DTaP/IPV/Hib/HepB vaccine, helps protect your child against:
What’s pertussis (whooping cough)?
Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. Whooping cough can last for up to 10 weeks.
Babies under one year old are most at risk from whooping cough. For these babies, the disease is very serious and can kill. It’s not usually as serious in older children. Before the pertussis vaccine was introduced, on average 120,000 cases of whooping cough were reported each year in the UK.
What’s diphtheria?
Diphtheria is a serious disease that usually begins with a sore throat and can quickly cause breathing problems.
It can damage the heart and nervous system and, in severe cases, can kill. Before the diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria a year, causing around 5,000 deaths.
What’s tetanus?
Tetanus is a disease affecting the nervous system that can lead to muscle spasms, cause breathing problems and even kill. It’s caused when germs that are found in soil and manure get into the body through open cuts or burns.
Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of the muscles. If it affects the chest muscles or the brain, polio can kill.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic. Because of the continued success of the polio vaccination, there have been no cases of paralytic polio in the UK for nearly 40 years (the last case was in 1984). Polio remains a threat with poliovirus traces found in London sewage in early 2022.
Being fully vaccinated is the best way to protect against becoming ill from polio. It’s important to make sure you and your child are up to date with your vaccines.
What’s Hib?
Hib is an infection caused by haemophilus influenzae type b bacteria. It can lead to a number of major illnesses such as blood poisoning (septicaemia), pneumonia and meningitis. The illnesses caused by Hib can kill if they’re not treated quickly. Before the Hib vaccine was introduced, there were about 800 cases of Hib in young children every year in the UK.
The Hib vaccine only protects your baby against the type of meningitis caused by the haemophilus influenzae type b bacteria – it doesn’t protect against any other type of meningitis.
More about haemophilus influenzae type b (Hib)
What’s hepatitis B?
Hepatitis B (HepB) is a virus that infects the liver. Many people with HepB infection have no symptoms and don’t know they’re infected. Others have flu-like symptoms and yellowing of the skin (jaundice).
In children, HepB can persist for years and may eventually cause serious liver damage.
Why should my baby be vaccinated?
Babies can catch these serious diseases from birth, so it’s important to protect them as soon as possible.
When will my baby be immunised?
All babies are eligible for the vaccine free on the NHS.
Your baby will be offered the 6-in-1 vaccine around 8, 12 and 16 weeks of age. Your local NHS immunisation team will contact you to let you know about their arrangements for your baby’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation baby clinics. If you can’t get to the clinic, contact your local NHS immunisation team to make another appointment.
Meningitis B (MenB) vaccine
Overview
The meningitis B (MenB) vaccine helps protect against meningitis and septicaemia (blood poisoning) caused by meningococcal bacteria B.
What’s meningitis?
Meningitis is inflammation of the lining of the brain and spinal cord. This causes pressure on the brain resulting in symptoms like:
- severe headache
- stiff neck
- dislike of bright light
- drowsiness
- convulsions/fits
Meningitis can progress very rapidly and can lead to:
- deafness
- blindness
- epilepsy
- learning difficulties
It can even lead to death.
What’s septicaemia (blood poisoning)?
Septicaemia (blood poisoning) is a serious, life-threatening infection that gets worse very quickly. The risk of death is higher compared to meningitis.
The signs of cold hands and feet, pale skin, vomiting and being very sleepy or difficult to wake can come on quickly.
More about meningitis and septicaemia
Charlotte’s story: meningococcal septicaemia (MenB)
Charlotte developed septicaemia (serious blood poisoning) through type B meningococcal disease (MenB) in 2010, before the MenB vaccine was introduced in the UK. Her mother Jenny talks about the impact on Charlotte and the rest of her family.
How common is type B meningoccocal disease?
MenB is now the cause of most cases of meningococcal disease in Scotland. Although this infection isn’t common, MenB is extremely serious and can lead to permanent disability and death. The meningococcal bacteria can also cause local outbreaks in nurseries, schools and universities.
Why should a baby be vaccinated?
MenB infection is most common in babies and young children. This is because their immune systems aren’t yet fully developed to fight off infection. The highest number of cases are in babies around 5 months of age. This is why the first immunisations are offered to babies younger than this and have to be given at 2 and 4 months of age.
This vaccine helps protect babies against MenB, There are other vaccines, like MenC, that protect against some other types of meningococcal infections.
Who is eligible for the vaccine?
The MenB vaccine is routinely offered to all babies at 8, 16 weeks, and 12 to 13 months.
When will a baby be immunised?
The MenB vaccine has been part of the routine childhood immunisation programme in Scotland since 1 September 2015. Your local NHS immunisation team will send you an appointment to bring your child in for their routine childhood immunisations.
Babies will be offered the MenB vaccine when they come in for their other routine immunisations at 8, 16 weeks and 12 to 13 months.
Find out how to contact your local NHS immunisation team regarding your vaccination appointment
If a baby is due their MenB vaccine, please ask your pharmacist about paracetamol for them. Fever can be expected after any vaccine but is more common when the MenB vaccine is given with the other routine immunisations at 8 and 16 weeks of age. This is why it’s recommended that babies gets infant paracetamol when getting these immunisations to prevent and treat fever.
Rotavirus vaccine
Overview
The rotavirus vaccine helps protect babies against rotavirus.
What’s rotavirus?
Rotavirus is a virus that infects the gut (tummy), causing severe diarrhoea and vomiting. Most babies get sick (vomit) or have diarrhoea at some time and recover fully after a few days. However, sickness and diarrhoea caused by rotavirus can lead to dehydration (loss of body fluids). Dehydration can be very dangerous for babies and young children and can require hospital treatment.
Before the vaccine was introduced in 2013, around 1200 babies in Scotland had to go to hospital every year with rotavirus.
Why should a baby be vaccinated?
The rotavirus immunisation protects a baby against this illness.
The most important thing you can do is have the baby immunised against rotavirus, as part of the Routine Childhood Immunisation Programme in Scotland.
In countries where babies already get the rotavirus vaccine there’s been a big drop in the number of babies and young children going to hospital because of the virus.
With lots of younger babies having the immunisation the chances of it spreading are reduced. Rotavirus causes fewer problems in older children, and it’s rare in adults.
When will a baby be immunised?
The rotavirus immunisation is offered to all babies in Scotland.
The rotavirus vaccine is normally given with the baby’s other routine immunisations at 8 weeks and again at 12 weeks of age. Your local NHS immunisation team will invite you for the vaccination, so there’s no need to book an appointment.
Pneumococcal vaccine for babies
Overview
The pneumococcal vaccine helps protect against illnesses and conditions caused by pneumococcal bacteria.
What illnesses and conditions are caused by pneumococcal bacteria?
Pneumococcal infection is caused by pneumococcal bacteria. It can cause serious illness such as pneumonia, and is one of the most common causes of meningitis (an infection of the lining of the brain).
Pneumococcal infection can cause:
- bronchitis
- ear and sinus infections
- a life-threatening infection of the blood (septicaemia)
- meningitis
- pneumonia (which can also be life-threatening).
Children under 2 years of age and children with certain health conditions have a higher chance of becoming unwell with pneumococcal infection.
How common are pneumococcal bacteria?
Up to 60% of children carry pneumococcal bacteria in the back of their nose and throat. They constantly pass these bacteria around by coughing, sneezing and close contact.
Why should a baby be vaccinated?
The pneumococcal vaccine provides some protection against meningitis caused by pneumococcal infection, and against other conditions such as severe ear infections and pneumonia caused by pneumococcal bacteria.
This vaccine doesn’t protect against meningitis caused by other bacteria or viruses.
Who is eligible for the vaccine?
Some children are at an increased risk from pneumococcal infection. All at risk children will be offered the vaccine according to the routine childhood immunisation programme. If you aren’t sure about your child’s health or need further advice, speak to your health professional.
When will a baby be immunised?
If a baby is eligible, they will be offered the pneumococcal vaccine when they’re 12 weeks old, with a booster dose given between 12 and 13 months. The pneumococcal booster dose between 12 and 13 months is usually given at the same time as the Hib/MenC, MMR and MenB vaccines.
In addition to this some children and adults aged from 2 to 64 years old, who are at a higher risk of developing a pneumococcal infection than the general population, will be offered additional pneumococcal vaccinations.
Your local NHS immunisation team will contact you to let you know about their arrangements for the baby’s routine childhood immunisations.
Hib Men C
Overview
The Hib/MenC vaccine helps protect a child against 2 of the causes of meningitis and septicaemia (blood poisoning). This vaccine will help protect the child through early childhood.
What is Hib?
Hib is an infection caused by Haemophilus influenzae type b bacteria. It can lead to a number of major illnesses such as septicaemia (blood poisoning), pneumonia and meningitis.
More about Haemophilus influenzae type b
What is meningitis?
Meningitis is inflammation of the lining of the brain and spinal cord. This causes pressure on the brain resulting in symptoms like:
- severe headache
- stiff neck
- dislike of bright light
- drowsiness
- convulsions/fits
Meningitis can progress very rapidly and can lead to:
- deafness
- blindness
- epilepsy
- learning difficulties
It can even lead to death.
What is septicaemia?
Septicaemia (blood poisoning) is a serious, life-threatening infection that gets worse very quickly. The risk of death is higher than with meningitis.
The signs of cold hands and feet, pale skin, vomiting and being very sleepy or difficult to wake can come on quickly.
Why should a baby be vaccinated?
A child will be offered a dose of the combined Hib/MenC vaccine between 12 and 13 months of age to:
- boost their protection against Haemophilus influenzae type b (Hib)
- help protect against meningitis and septicaemia caused by meningococcal group C (MenC) bacteria
The Hib/MenC vaccine doesn’t protect against meningitis and septicaemia (blood poisoning) caused by:
- meningococcal group B bacteria
- other bacteria or viruses such as pneumococcal or mumps
When will a baby be immunised?
A baby will be offered the Hib/MenC vaccine at 12 to 13 months. Your local NHS immunisation team will contact you to let you know about their arrangements for the baby’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation baby clinics. If you cannot attend your appointment contact your NHS immunisation team to make another.
Find out how to contact your NHS immunisation team regarding the baby’s vaccination appointment
MMR
The MMR vaccine is given in 2 doses and helps protect against measles, mumps and rubella. Find out more about the vaccine, and when and where to get it.
Why should someone have the MMR vaccination?
The MMR vaccine helps to protect people against measles, mumps and rubella. It’s sometimes also offered to adults who missed their childhood immunisations.
Measles, mumps and rubella are highly infectious diseases. They can cause serious medical complications.
A high number of people in Scotland have had the MMR vaccine. This means there’s been a big reduction in the number of people catching these diseases.
Who is eligible for the MMR vaccine?
All babies and children in Scotland are eligible for the MMR vaccine.
They’ll be offered the MMR vaccine in 2 doses:
- the first between 12 and 13 months
- the second at 3 years 4 months
Although normally given at these times, if it’s missed, it can be given at any age.
Some young people and adults who missed out on their MMR vaccine may also be eligible, like those who are a planning a pregnancy. If you didn’t have 2 doses of the MMR vaccine as a child, you can contact your local NHS immunisation team to discuss your eligibility.
The 4-in-1 Vaccine
Overview
The 4-in-1 vaccine, also known as the DTaP/IPV or dTaP/IPV vaccine, helps protect your child against:
- pertussis (whooping cough)
- diphtheria
- tetanus
- polio
What’s pertussis (whooping cough)?
Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. Whooping cough can last for up to 10 weeks.
Babies under one year are most at risk from whooping cough. For these babies, the disease is very serious and can kill. It’s not usually as serious in older children.
Whooping cough germs can be spread from person to person through close contact.
What’s diphtheria?
Diphtheria’s a serious disease that usually begins with a sore throat and can quickly cause breathing problems. It can damage the heart and nervous system and, in severe cases, can kill.
Diphtheria germs are spread from person to person through close contact.
What’s tetanus?
Tetanus is a disease affecting the nervous system that can lead to muscle spasms, cause breathing problems and even kill.
It’s caused when germs found in soil and manure get into the body through open cuts or burns. Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of the muscles. If it affects the chest muscles or brain, polio can kill.
The polio virus is usually spread from person to person, or by swallowing contaminated food or water.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic. Because of the continued success of the polio vaccination, there have been no cases of paralytic polio in the UK for nearly 40 years (the last case was in 1984). Polio remains a threat with poliovirus traces found in London sewage in early 2022.
Being fully vaccinated is the best way to protect against becoming ill from polio. It’s important to make sure you and your child are up to date with your vaccines.
Why should my child be vaccinated?
The vaccine boosts the immunisations that were given to your child at 8, 12 and 16 weeks of age – boosting protection against pertussis (whooping cough), diphtheria, tetanus, and polio.
Who is eligible for the vaccine?
This vaccine’s offered to children aged over 3 years 4 months at the same time as they are offered the MMR vaccine. It’s also used for a primary course of immunisation in children over 10 years old and adults.
When will my child be immunised?
Your child will be offered the 4-in-1 vaccine at around 3 years and 4 months. Your local NHS immunisation team will contact you to let you know about their arrangements for your child’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation clinics. If you can’t get to the clinic, contact your local NHS immunisation team to make another appointment.
Young people in Secondary School/not in mainstream education
HPV Vaccine – S1 to S6
What the HPV vaccine is for
Immunisation (vaccination) information in other languages
Evidence shows the HPV vaccine helps protect people from HPV-related cancers. The human papillomavirus (HPV) vaccine is offered to every S1 pupil in Scotland.
Getting the vaccine now protects you against future risks. HPV can lead to cancers like:
- head and neck cancers
- cervical cancer
- anogenital cancers – for example, anal, penile (penis) cancer, cancer of the vagina, and cancer of the vulva
The HPV vaccine also protects you against over 90% of genital wart infections.
Who can get the HPV vaccine
Every person in Scotland aged 11-13 will be offered the HPV vaccine free of charge.
You should not have some vaccines if you’ve had a confirmed serious (anaphylactic) reaction to:
- a previous vaccine
- any ingredient of the vaccine
About the HPV vaccine
The GARDASIL 9 vaccine is used in Scotland.
Gardasil 9 helps protect against 9 types of HPV.
The vaccine protects against HPV types 16 and 18, which are the cause of most cervical cancers in the UK (more than 80%). The vaccine also protects against types 31, 33, 45, 52 and 58, which cause an additional 15% of cervical cancers.
The vaccine also protects against 2 other types of HPV. These cause around 90% of cases of genital warts.
The HPV vaccine is not a live vaccine. It cannot cause HPV.
The vaccine is the safest and most effective way to protect against HPV.
How to get the HPV vaccine
You’ll be offered the HPV vaccine as part of the school-based immunisation programme. Vaccines are given by your local NHS immunisation team.
Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you missed your vaccination and you’re still at school
If you miss your HPV vaccination, there will be further opportunities to get it. For example, you may be offered a rescheduled vaccination appointment next year.
If you’re unsure if you’ve missed any other vaccines, you should
first check your red book. If you do not have a red book, or it has gone missing, you can check with your local NHS immunisation team.
Young people not in mainstream education
You’re also eligible for the HPV vaccine if you’re:
- educated at home
- not in mainstream education
Please contact your local NHS immunisation team to arrange your appointment.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
If you’ve missed your vaccination and have now left school
If you’ve left school and you didn’t get your HPV vaccine when you were eligible, you may still be able to get it up until you turn 25.
This only applies to:
- people who are currently eligible
- boys who became eligible from the 2019/2020 academic year
- girls under 25 who were eligible under routine and catch up programmes introduced in 2008
Your local NHS immunisation team can confirm if you’re eligible. They can also explain how to get the HPV vaccine in your area.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
The vaccine consent form
You should be given a consent form and leaflet by your school. You and your parent or carer should chat about the information. Both you and your parent or carer should sign the consent form and return it to your school. You should return the consent form even if you’re not going to have the vaccine.
We recommend you get agreement from your parent or carer, but it isn’t always necessary.
MMR Vaccine – S1 – S6
The MMR vaccine is given in 2 doses and helps protect against measles, mumps and rubella. Find out more about the vaccine, and when and where to get it.
Why should someone have the MMR vaccination?
The MMR vaccine helps to protect people against measles, mumps and rubella. It’s sometimes also offered to adults who missed their childhood immunisations.
Measles, mumps and rubella are highly infectious diseases. They can cause serious medical complications.
A high number of people in Scotland have had the MMR vaccine. This means there’s been a big reduction in the number of people catching these diseases.
Who is eligible for the MMR vaccine?
All babies and children in Scotland are eligible for the MMR vaccine.
They’ll be offered the MMR vaccine in 2 doses:
- the first between 12 and 13 months
- the second at 3 years 4 months
Although normally given at these times, if it’s missed, it can be given at any age.
Some young people and adults who missed out on their MMR vaccine may also be eligible, like those who are a planning a pregnancy. If you didn’t have 2 doses of the MMR vaccine as a child, you can contact your local NHS immunisation team to discuss your eligibility.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
DTP Vaccine – S3 to S6
The DTP vaccine provides protection against diphtheria, tetanus and polio. The vaccine is usually given in S3 (around 14 years old). Find out when and where to get it.
What the DTP vaccine is for
Immunisation (vaccination) information in other languages and formats
The DTP vaccine protects against diphtheria, tetanus and polio. These are serious diseases.
You need a total of 5 doses of the diphtheria, tetanus and polio vaccine to build up immunity and give you longer-term protection.
You should have had:
- the first 3 doses as a baby
- the fourth dose before you started primary school (after turning 3 years and 4 months)
You should have the fifth dose in S3 (around 14 years old).
What’s diphtheria?
Diphtheria is a serious disease that usually begins with a sore throat. It can quickly cause breathing problems. It can also damage the heart and nervous system, and in severe cases, can kill. Diphtheria is passed from person to person through close contact.
Before the diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria a year. These caused around 5,000 deaths.
What’s tetanus?
Tetanus is a painful disease affecting the nervous system that can lead to:
- muscle spasms
- breathing problems
- death
It’s caused by germs found in soil and manure getting into the body through open cuts or burns.
Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of muscles. If it affects the chest muscles or the brain, polio can kill. The polio virus is usually spread from person to person or by swallowing contaminated food or water.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic.
Who can get the DTP vaccine
All young people in S3 (around 14 years old) are eligible for the vaccination. This is part of their routine immunisation schedule.
- If you were immunised as a child – The DTP vaccine completes the 5 dose course against diphtheria, tetanus and polio. Although you’ve already had 4 doses of diphtheria, tetanus and polio vaccines, , you need a total of 5 to build up your immunity and provide longer-term protection.
- Reasons you should not have the vaccine – here are very few young people who can’t have the DTP vaccine. You shouldn’t have the vaccine if you’ve had a confirmed anaphylactic reaction to:
- a previous vaccine
- any ingredient of the vaccine
- neomycin, streptomycin or polymyxin B (antibiotics that may be added to vaccines in very tiny amounts)
- If you have a bleeding disorder – If you have a bleeding disorder, tell the person giving you the vaccine. They’ll give the injection in a slightly different way that will be better for you.
About the DTP vaccine
The REVAXIS vaccine is routinely used in Scotland.
The DTP vaccine is not a live vaccine. It cannot cause the diseases it protects against.
The DTP vaccine is the safest and most effective way to protect against serious diseases.
How to get the DTP vaccine
You’ll be offered the DTP vaccine when you’re in S3 (around 14 years of age) at school. Vaccines are given by your local NHS immunisation team. Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
Meningitis ACWY (MenACWY) vaccine – S3 to S6
The meningitis ACWY (MenACWY) vaccine helps protect against meningitis and septicaemia (blood poisoning). Find out more about the MenACWY vaccine, and when and where to get it.
What the Meningitis ACWY (MenACWY) vaccine is for
Immunisation (vaccination) information in other languages and formats
The meningitis ACWY (MenACWY) vaccine helps protect against meningitis and septicaemia (blood poisoning), which are caused by meningococcal bacteria A, C, W and Y.
Young people have a higher risk of getting meningococcal disease. You’ll be offered immunisation to protect yourself and others around you.
Meningitis and septicaemia are very serious diseases. They can cause permanent disability and death. The symptoms can come on quickly.
Who can get the MenACWY vaccine
The MenACWY vaccine is routinely offered to all young people in S3 (around 14 years of age). If you’re over 14 and not already immunised, you may also be offered the vaccine.
You should not have some vaccines if you’ve had a confirmed anaphylactic shock (serious allergic reaction) to:
- a previous vaccine
- any ingredient of this vaccine
About the MenACWY vaccine
The following vaccines are routinely used in Scotland:
- Menveo Meningococcal Group A, C, W135 and Y conjugate vaccine
- Nimenrix powder and solvent for solution for injection in pre-filled syringe
The MenACWY vaccine is highly effective at protecting against the serious infections caused by meningococcal bacteria A, C, W and Y.
The MenACWY vaccine is not a live vaccine. It cannot cause meningitis.
The MenACWY vaccine is the safest and most effective way to protect against meningococcal A, C, W and Y.
How to get the MenACWY vaccine
Vaccines are given by your local NHS immunisation team. Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you missed your vaccination at school
If you missed your MenACWY vaccination, there will be further opportunities to get it. For example, you may be offered a rescheduled vaccination appointment next year.
If you’re unsure if you’ve missed any other vaccines, you should first check your red book. If you do not have a red book, or it has gone missing, you can check with your local NHS immunisation team
Young people not in mainstream education
You’re also eligible for the MenACWY vaccine if you’re:
- educated at home
- not in mainstream education
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
Students
You may be eligible for the MenACWY vaccination if you:
- are Scottish and attending further education in Scotland
- are aged up to 25 years old
- have not had the MenACWY vaccination
You should contact your local NHS immunisation team. They’ll advise you if it’s clinically appropriate for you to have the vaccine.
You may not be eligible for the MenACWY vaccination if you’re from outside Scotland (including other parts of the UK). You should arrange to get your vaccine before travelling to Scotland. There’s no guarantee the vaccine will be available to you after arriving in Scotland.
Seasonal Vaccination
Pre-School 6 Months to 2 Years at Risk – Flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
Children aged 6 months to 2 years will be given the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Pre-School 6 Months to 4 Years at Risk – Covid
NHS Scotland is offering the coronavirus (COVID-19) vaccine to children aged 6 months to 11 years at higher risk of coronavirus this spring.
To be invited for vaccination this spring, your child must have a weakened immune system and be aged 6 months to 11 years on 31 March 2024 (born on or after 1 April 2012 and before 1 October 2023).
Why is my child being offered the coronavirus vaccine?
Getting the vaccine will help to protect your child against coronavirus. The vaccine helps to build up immunity to coronavirus, so the body can fight it off more easily. If your child is vaccinated, they are much less likely to get seriously ill from coronavirus or need to go to hospital.
Infants and young children with underlying health conditions are 7 times more likely to be admitted to paediatric intensive care units with severe coronavirus, compared to those without underlying health conditions.
My child has already had the coronavirus vaccine – do they need another one?
NHS Scotland is offering a coronavirus vaccine to children at higher risk to help protect them this spring. It’s important to keep up to date with the coronavirus vaccines your child is offered.
NHS Scotland recommends coming forward every time your child is invited to keep their protection topped up.
Is the coronavirus vaccine safe?
NHS Scotland will only use a vaccine if it meets the required standards of safety and effectiveness. All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used. The Medicines and Healthcare products Regulatory Agency (MHRA) assesses all the data and also ensures a vaccine works and that all the necessary trials and checks have been completed.
Are there any reasons my child should not get the coronavirus vaccine?
There are very few people who cannot have the vaccine. If your child has had a confirmed severe allergic reaction (anaphylaxis) to any of the vaccine ingredients or a previous dose of the same vaccine, you should seek advice from your health professional before your child has the vaccine.
The vaccine is not a live vaccine and does not contain any animal products or egg.
Vaccine manufacturer patient information leaflets
More information about the vaccines offered, including vaccine ingredients, is available in the manufacturer patient information leaflets.
Read the coronavirus vaccine patient information leaflet for 6 months to 4 years:
Pre-School 2 – 5 year old childhood flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
The flu vaccine is available between September and March.
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu. Children aged 2 to 5 are being offered vaccination from the start of the programme to ensure they receive the earliest protection and prevent the virus spreading.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
In Scotland, children aged 2 to 17 will usually be given the nasal spray flu vaccine. It’s quick and painless and there’s no need to sniff or inhale the vaccine. It’ll just feel like a tickle in their nose.
Children aged 2 to 17 years who cannot receive the nasal spray vaccine will receive the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Primary School Children – Flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
The flu vaccine is available between September and March.
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu.
Consent forms and further information will be sent home to parents and carers of school children on return to school. Secondary pupils can self-consent but are encouraged to speak to a parent or carer first. All primary and secondary school pupils with consent to be given the flu vaccine nasal spray will receive this at school starting in early September through to December 2024.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
In Scotland, children aged 2 to 17 will usually be given the nasal spray flu vaccine. It’s quick and painless and there’s no need to sniff or inhale the vaccine. It’ll just feel like a tickle in their nose.
Children aged 2 to 17 years who cannot receive the nasal spray vaccine will receive the injectable flu vaccine.
Children aged 6 months to 2 years will be given the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Where clinics take place
Vaccinations are typically given in schools during term time. NHS GGC work with schools to communicate programme dates.
Before clinics take place, consent forms and vaccination information will be handed out to pupils at school for review at home then return to school.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
On the day
Pupils will usually attend clinics in the school hall or social space, class by class throughout the day.
Secondary School Children and Young People – Flu
About the programme
Immunisation is the safest and most effective way of protecting young people against serious diseases.
School-aged children are routinely vaccinated against:
- Influenza – usually offered to all primary and secondary school pupils from September to December .
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu.
Consent forms and further information will be sent home to parents and carers of school children on return to school. Secondary pupils can self-consent but are encouraged to speak to a parent or carer first. All primary and secondary school pupils with consent to be given the flu vaccine nasal spray will receive this at school starting in early September through to December 2024.
https://www.nhsinform.scot/vaccineconsentyoungpeople
For details of the schedule of vaccinations in Scotland by age, please refer to NHS Inform.
Where clinics take place
Vaccinations are typically given in schools during term time. NHS GGC work with schools to communicate programme dates.
Before clinics take place, consent forms and vaccination information will be handed out to pupils at school for review at home then return to school.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
On the day
Pupils will usually attend clinics in the school hall or social space, class by class throughout the day.
FAQs
I am unsure of my child’s immunisation history
Please contact your GP
Pre-School Team Contact Details
Please see team contact details below:
Glasgow South/East Renfrewshire
Phone Number: 0141 577 7774 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Castlemilk, Eastwood, Govanhill, Gorbals, Govanhill (EU), Pollock, Shields Centre, Elderpark, Thornliebank, Barrhead
North East/East Dunbartonshire
Phone Number: 0141 531 6635 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Springburn, Kirkintilloch, Stobhill, Milngavie, Baillieston, Shettleston, Bridgeton, Townhead, Easterhouse
North West/West Dunbartonshire
Phone Number: 0141 211 6142 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Dumbarton, Vale of Leven, Maryhill, Woodside, Possilpark, Community Centre for Health (CCFH), Plean Street, Drumchapel, Clydebank
Renfrewshire/Inverclyde
Phone Number: 0141 201 1056 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Greenock, Port Glasgow, Johnstone, Linwood, Renfrew, Foxbar Clinic, Northcroft, Tannahill Centre, Erskine
School Team Contact Details
Please see team contact details below:
Glasgow South/East Renfrewshire
Phone Number: 0141 577 7767 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
North East/East Dunbartonshire
Phone Number: 0141 232 9838 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
North West/West Dunbartonshire
Phone Number: 0141 232 9202 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Renfrewshire/Inverclyde
Phone Number: 0141 314 0513 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Was this helpful?
It is important that you seek an appointment in plenty of time before you travel. We advise you to contact our services at least 8 weeks before your travel date. This will allow us to accommodate your needs and ensure you are fully protected before you go.
We may not be able to accommodate you at short notice. In this instance, we will suggest that you seek an appointment with one of the many private providers operating across Greater Glasgow and Clyde.
Why should you get your vaccinations
With many people travelling more frequently and to more far flung destinations the risk of disease and illness are more likely – even if you are visiting family and friends or were born in the country you are travelling too. It is important that you are protected against these diseases E.g. Typhoid Fever/Hepatitis A so that you do not become ill on your return and require hospital admission. The vaccines protect you against these illnesses.
Proof of Vaccination
It is helpful to carry a record of your vaccinations. Generally this is not required, however, some countries do require proof of Polio and other vaccines such as Yellow Fever. When you are seen by our Clinic and are travelling to a country which requires proof on exit you will be provided with an International Certificate of Vaccination (ICVP). It is essential you have this with you otherwise the country you are visiting may either not let you enter the country or revaccinate you prior to leaving the country E.g. Pakistan evidence required of Polio on exit.
Yellow fever vaccines are only available from designated centres. To find out if you need a yellow fever vaccine or proof of yellow fever vaccine, you should contact a designated yellow fever clinic. You can download a PDF copy of your COVID Status online or phone the COVID Status helpline on 0345 034 2456.
Costs and Payment
There is no charge for your risk assessment/consultation and the following vaccinations are provided free on the NHS: Diptheria, Tetanus and Polio (DTP), Typhoid, Hepatitis A and Cholera. However, there is a charge for some other vaccines and services.
At your appointment, you will be offered vaccines based on your individual risk assessment, the country you are travelling to and the type of travel you are undertaking.
You can find local travel clinics via the NHS inform website:
Was this helpful?
Information on all the vaccinations available, including general child and adult ones, COVID, flu and travel.
Was this helpful?
There has been a significant increase in travelling over the last decade or so with many of us travelling to more far flung destinations. As a result there has been an increase in preventable travel related illness.
If you’re visiting friends or family, backpacking on your gap year or heading off on a family holiday, you may require a Travel Health Assessment and also vaccinations to keep you safe. Many vaccinations are available for free on the NHS.
GP’s previously delivered travel health vaccines however, this service is now provided by your health board. To get the care and advice you need it is important that you seek an appointment in plenty of time before you travel.
We advise you to contact our services at least 8 weeks before your travel date.
Making an appointment
NHS GGC Travel Health Services
- Email: Ggc.VaccinationContactCentre@ggc.scot.nhs.uk
- Call: 0800 9176115
- New Address – Parkview Resource Centre: 152 Wellshot Rd, Glasgow G32 7AX
- Opening date – 17th March 2025
- Contact details – Booking line: 0800 917 6115
- Emcare remains our preferred partner for additional vaccines not available on the NHS.
- Parking – both on site (limited) and on road parking available – 2 disabled parking spaces on site and venue has ramp access and disabled toilets.
- Transport links – Carntyne station (0.5 miles / 15 mins walk)
- Bus route – Shettleston road & Toll cross road buses
- You can plan your journey by going to Traveline Scotland Journey Planner: Traveline Scotland |
Health Professionals Providing Travel Health Advice
Prior to travel, UK residents planning to undertake Hajj or Umrah should be advised to:
- Check with a travel health professional as early as possible to identify what vaccines or boosters are required before travelling to Hajj/Umrah. MenACWY vaccine is required at least 10 days prior to travel as part of the Hajj/Umrah visa. It is recommended that travellers have received two doses of MMR vaccine.
- Follow the Foreign, Commonwealth and Development Office (FCDO) travel advice for Saudi Arabia.
- Follow official Kingdom Saudi Arabia Ministry of Hajj and Umrah guidance by registering and booking through the Nusuk Hajj website.
- Obtain comprehensive travel insurance before travelling for Hajj and Umrah.
Returning Travellers
Returning travellers from Saudi Arabia are advised to call their GP by phone or call NHS24 on 111 (out of hours) as soon as possible if experiencing flu-like symptoms (including fever, cough and/or shortness of breath) within 14 days of returning from Saudi Arabia, mentioning their recent travel.
This service is only for those residing within the NHSGGC Health Board area.
Attending your appointment
Please bring a note of your vaccination history with you to your appointment
If you are unable to provide this information at the time of your appointment it may cause a delay in you receiving any necessary vaccinations and you may have to return at a later date. If you have children attending with you, please bring the child’s red book or details of any vaccinations the child has received in school.
You must give a minimum of 48 hours notice of cancellation
If you have an appointment to receive your travel vaccinations and are no longer able to attend, it is important you tell us as early as possible. Late cancellation or not attending your appointment result in a cost to the NHS and denies others the opportunity to receive an NHS travel health appointment.
Covid Vaccination
We will not vaccinate you with Covid-19 unless this is a requirement for entry for a country you are travelling too. There are very low numbers of countries that require this now and information on the up to date list can be found on the Government website for the country you are travelling to.
A current list of countries that require Covid-19 vaccination for travel entry certification purposes can be found here: COVID-19 Vaccination Requirements.
If you require covid vaccination for entry and haven’t had your primary course, please get in touch with the contact centre on 0800 917 6115 who will arrange an appointment.
Get advice about travelling abroad, including the latest information on coronavirus, safety and security, entry requirements and travel warnings:
Hajj and Umrah Pilgrimage
Routine Vaccines
Before travelling to Hajj or Umrah it is recommended that you are up-to-date with routine vaccines for life in the UK, including:
- diphtheria, tetanus and polio
- a minimum of 5 doses of a diphtheria, tetanus and polio-containing vaccine are needed in your lifetime to provide good long-term protection.
- measles, mumps and rubella (MMR)
- two doses of MMR vaccine are needed in your lifetime to protect you against all three viruses
- seasonal flu (influenza) if you are eligible
- see NHS inform and NHS UK for more information on the UK flu vaccine campaigns
- MenACWY vaccine at least 10 days prior to travel as part of the Hajj/Umrah visa.
Before you Travel
Before booking travel, check the ‘Entry Requirements’ section of the Foreign Commonwealth and Development Office (FCDO) guidance for the latest rules you will need to comply with to enter the Kingdom of Saudi Arabia (KSA).
Travel Insurance
You should purchase comprehensive travel insurance before travelling:
- make sure you tell your travel insurance company about any existing health conditions; if you don’t they may not cover you if you get sick
- see the travel insurance page for more information
Get advice about travelling abroad, including the latest information on coronavirus, safety and security, entry requirements and travel warnings:
Further Information
Was this helpful?
Older Adult Vaccinations
Pneumococcal Vaccine
Overview
The pneumococcal vaccine provides some protection against illnesses caused by pneumococcal bacteria.
What are pneumococcal bacteria?
Pneumococcal bacteria cause pneumococcal infection. They can cause serious illnesses like pneumonia and bacterial meningitis. They can also cause other conditions like severe ear infections.
Some adults carry pneumococcal bacteria in the back of their nose and throat. They can pass bacteria on by coughing, sneezing, and close contact.
Exposure to pneumococcal bacteria doesn’t normally result in serious illness. But, sometimes it leads to pneumococcal infections.
You have a higher chance of becoming unwell with a pneumococcal infection if:
- you’re aged 65 or over
- you’re under 65 and have certain health conditions
People aged 65 or over are more likely to suffer serious long-term health problems from pneumococcal infection. These health problems can lead to death.
What is pneumococcal disease and why do we need a vaccine?
Dr Andrew Prendergast explains why it’s important to vaccinate against pneumococcal disease.
Why should I be vaccinated?
The pneumococcal vaccine provides some protection against the serious conditions caused by pneumococcal bacteria. These conditions include:
- one of the most common types of meningitis
- severe ear infections
- pneumonia caused by pneumococcal bacteria
This vaccine doesn’t protect against meningitis or pneumonia caused by other bacteria or viruses.
Who is eligible for the vaccine?
The pneumococcal vaccine is available in Scotland for all people aged 65 and over.
Some people under 65 are also eligible for the vaccine if they have certain health conditions, or are at high risk of exposure because of their job. You may be at risk if you have:
Asplenia or problems with the spleen
This includes conditions that can lead to problems with the spleen, like homozygous sickle cell disease or coeliac syndrome.
Read more about vaccinations for those with problems with their spleen (asplenia)
Chronic respiratory disease
This includes:
- chronic obstructive pulmonary disease (COPD)
- chronic bronchitis
- emphysema
- bronchiectasis
- cystic fibrosis
- interstitial lung fibrosis
- pneumoconiosis
- bronchopulmonary dysplasia
- asthma, if it’s so severe that you need constant or repeated use of systemic steroids
Chronic heart disease
This includes conditions like:
- ischaemic heart disease
- congenital heart disease
- hypertension with cardiac complications
- chronic heart failure
Chronic liver disease
This can include:
- cirrhosis
- biliary atresia
- chronic hepatitis
Chronic kidney disease
This can include:
- nephrotic syndrome
- chronic kidney disease at stages 4 and 5
- those on kidney dialysis
- those who’ve had a kidney transplant
Diabetes
If you’ve diabetes and use insulin or anti-diabetic medication, you’re eligible for extra pneumococcal vaccinations.
If your diabetes is controlled by diet and you’re under 65 years old, you’re not eligible for extra pneumococcal vaccination.
If you’re over 65 years old, you’re eligible for your pneumococcal vaccination regardless of how your diabetes is controlled.
Immunosuppression
People who are immunosuppressed may be offered extra pneumococcal vaccines. These people include patients who:
- are having chemotherapy
- have had a bone marrow transplant
- have asplenia or problems with their spleen
- have complement disorder
- have HIV infection (at any stage)
- have multiple myeloma
- have a genetic disorder that affects the immune system, like IRAK-4 or NEMO
- are on or are likely to be on a high dose of systemic steroids for more than a month
Cochlear implants
Individuals with cochlear implants are eligible for extra pneumococcal vaccinations
Cerebrospinal fluid leak
If you have leakage of cerebrospinal fluid from trauma or major skull surgery, you may be eligible for extra pneumococcal vaccinations.
This does not include leakage from CSF shunts, which deliberately drain excess fluid from the brain to another part of the body.
Occupational risk
Research has found a link between exposure to metal fumes and pneumonia.
If your job involves frequent or constant exposure to metal fumes, you may be considered at risk. This would make you eligible for the pneumococcal vaccine. An example of an at risk occupation would be a welder.
How do I get my pneumococcal vaccination?
You do not need to arrange your appointment. You’ll be contacted by your local NHS immunisation team when you’re eligible to be immunised. They’ll tell you:
- the date and time of your appointment
- where your appointment will be
They’ll contact you by sending an invitation to your home address. This is the address that is registered with your GP.
You can be invited for the vaccine at any time of the year.
Shingles Vaccine
Who is eligible for the shingles vaccine?
Your local NHS immunisation team will contact you when you’re eligible to get the vaccine. This will be from January 2024 onwards. Please wait to be contacted. Eligibility for the shingles vaccine depends on what age you were on 1 September 2023.
If you’re not sure if you’re eligible, you can use the age eligibility calculator to check.
Why should I have the shingles vaccine?
Shingles can be very painful and is more common among older people. The older you are, the worse it can be. For some, the pain caused by shingles can last for many years.
People who have a severely weakened immune system are also at higher risk of getting shingles and experiencing further complications from it.
Every year in Scotland, around 400 people aged 70 and over will be hospitalised due to shingles and related complications.
The shingles vaccine helps to build up your immunity to the virus. This means, if you do get shingles, your body will fight it off more easily.
Getting the vaccine will:
- reduce your risk of developing shingles by over 70%
- reduce your risk of experiencing long-term pain from shingles
- reduce your risk of being hospitalised with complications from shingles
What is shingles?
Shingles is caused by a virus called varicella zoster. This is the same virus that causes chickenpox. When you recover from chickenpox most of this virus is destroyed, but some of the virus survives and lies inactive in your body’s nervous system.
The virus can then become active again later in life. This normally happens when your immune system has been weakened by:
- age
- stress
- illness
- certain treatments that can reduce your immunity
The shingles vaccine helps to protect you by boosting your immunity.
More about the symptoms of shingles
Do I need the shingles vaccine if I’ve never had chickenpox?
Yes. The chances are that you may have had chickenpox at some point without knowing it. Some people have chickenpox without displaying any of the typical chickenpox symptoms.
Do I need the shingles vaccine if I’ve had shingles before?
Yes. Even if you’ve already had shingles, you should still get it again. The vaccine will reduce your risk of getting shingles again.
What vaccine will be offered?
From September 2023, the Shingrix vaccine will be used in Scotland.
You can view the vaccine ingredients in the Shingrix patient information leaflet.
Are there any reasons I shouldn’t have the shingles vaccine?
You shouldn’t have the shingles vaccine if you’ve had a severe allergic reaction (anaphylaxis) to:
- any of the ingredients in the vaccine
- a previous dose of the chickenpox vaccine
Is the shingles vaccine a live vaccine?
No, the shingles vaccine is not a live vaccine. It cannot cause shingles.
How many doses of the vaccine do I need?
You need to have 2 doses of the shingles vaccine for it to be effective.
You’ll be offered your second dose 2 to 12 months after your first dose.
How do we know the vaccine is safe?
The shingles vaccination programme was introduced in Scotland in 2013.
All medicines (including vaccines) are tested for safety and effectiveness. The vaccine meets the high safety standards required for it to be used in the UK and other European countries. The vaccine has been given to millions of people worldwide.
Once they’re in use, the safety of vaccines continues to be monitored.
Respiratory Syncytial Virus (RSV) Vaccine
The respiratory syncytial virus (RSV) vaccine helps to protect people from RSV.
RSV is a common respiratory (lungs and airways) illness. RSV infection is more common from late autumn to early spring, but can happen at any time of year.
Sometimes, RSV infection can cause severe lower respiratory infections like pneumonia. It can also cause other life-threatening conditions.
Last year in Scotland, there were over 1,000 RSV cases in adults aged 75 and over.
The vaccine helps protect you by reducing your chances of getting an RSV infection.
Who can get the RSV vaccine
If you’re turning 75 years old between 1 August 2024 and 31 July 2025, you’ll be offered the RSV vaccine. This includes if your 75th birthday is on 1 August 2024 or 31 July 2025.
The vaccine will also be offered to anyone who is aged 75 to 79 years on 1 August 2024. This means you can get the vaccine if your date of birth is between 2 August 1944 and 31 July 1950. This is because the RSV vaccine is new to Scotland, and this group could not be given the vaccine before now.
In future years, the vaccine will be routinely offered to those turning 75 years old between 1 August and 31 July.
Getting the RSV vaccine is the best way to protect yourself against infections caused by RSV.
About the RSV vaccine
The Abrysvo vaccine is offered to protect against RSV in Scotland. It’s usually given as an injection in your upper arm.
You may be able to get the RSV vaccine at the same time as other vaccines (like shingles or pneumococcal). You can discuss this with the person giving you the vaccine. Because RSV infections often happen earlier in the year, this vaccine will be offered in August and September. You’ll be offered a different appointment later in the year to get your flu vaccine.
The Abrysvo vaccine is not a live vaccine. It does not cause RSV infection.
Read more about vaccines for older adults
There are very few people who cannot have the RSV vaccine.
The vaccine should not be given to people who have had a severe allergic reaction (anaphylaxis) to:
- ny of the vaccine ingredients
- a previous dose of the same vaccine
You can view the ingredients in the Abrysvo vaccine patient information leaflet.
It’s important to tell the person giving you the vaccine if you:
- have ever had a severe allergic reaction (anaphylaxis) to anything
- are receiving medicines, treatment or therapy at a hospital or specialist clinic
How to get the RSV vaccine
You’ll be contacted by your local NHS immunisation team when it’s time to get the vaccine. Most immunisation teams will begin inviting patients from August 2024 onwards.
If you’re ill on the day of your appointment
Reschedule your vaccine appointment if you feel very unwell, for example if you have a fever, vomiting or diarrhoea. You should not attend an appointment if you think you might be infectious to others.
To reschedule your appointment, phone the number on your invitation letter. If you’ve lost your invitation letter, contact your local NHS immunisation team.
Side effects of the RSV vaccine
After having the vaccine you may have some side effects. These are usually mild and disappear within a few days.
Around the injection site you might experience:
- pain
- redness
- swelling
Where can I report side effects?
You can report suspected side effects of vaccines and medicines through the Yellow Card Scheme.
This can be done:
- via their website
- through the Yellow Card Scheme app
- by phoning 0800 731 6789 (9am to 5pm, Monday to Friday)
Flu Vaccine
Flu vaccine
Influenza (flu) is an infectious virus and can be serious. Symptoms may include a fever, a cough, a headache and tiredness. The virus spreads through the air when people cough or sneeze, or when they touch surfaces where the virus has landed then touch their eyes, nose or mouth. You can catch flu all year round, but it’s especially common in winter. It can be serious, even if you’re healthy.
The flu vaccine
The flu vaccine is the safest and most effective way to help protect against flu. It’ll also help reduce the risk of spreading flu to others.
The flu vaccine is available between September and March.
Why should I get vaccinated?
The flu vaccine has a good safety record. It gives the best protection against flu. It’s offered every year for free by the NHS to help protect people at risk of flu and its complications.
The vaccine helps protect against the main types of flu viruses. But there’s still a chance you might get flu after having the vaccine. If you do get flu, it’s likely to be milder and not last as long if you’ve received the flu vaccine.
Having the flu vaccine can also stop you spreading flu to other people who may be more at risk of complications and serious illness if they catch flu.
You have to get immunised every year because flu viruses change constantly and your immunity reduces over time.
The flu vaccine can’t give you flu, but it can stop you catching it.
Vaccine safety
All medicines (including vaccines) are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
Pregnant Women Vaccinations
Whooping Cough Vaccine
What the whooping cough vaccine is for
The whooping cough vaccine protects your baby against whooping cough.
Whooping cough (also known as pertussis) is a disease that can be very serious for babies. It’s a highly contagious bacterial infection that affects the lungs and airways. It can last for 2 to 3 months.
Babies and young children are at increased risk of complications from whooping cough. It can be very serious, and lead to pneumonia and permanent brain damage. In the worst cases, whooping cough can be life threatening.
Read more about whooping cough and its symptoms
Who can get the whooping cough vaccine
In Scotland, the whooping cough vaccine is offered to everyone who is pregnant.
If you’re pregnant, you’ll be offered the vaccine from week 16 of your pregnancy.
It’s better to get the whooping cough vaccine as soon as possible. The sooner you get the vaccine, the more time there is for you to pass antibodies to your baby.
When you get the whooping cough vaccine, your body makes antibodies. These are what your body uses to fight whooping cough. These antibodies will transfer from you to your unborn baby through the placenta. This means that your baby will have some protection from whooping cough as soon as they’re born.
The protection you receive from the vaccine will also lower your own risk of getting whooping cough and passing it to your baby.
Read more about the routine vaccinations offered to babies
If you’ve had whooping cough before
Even if you’ve had whooping cough before, you need the vaccine to help protect your baby.
Getting the whooping cough vaccine is the best way to protect your baby from whooping cough.
If you’ve had the whooping cough vaccine before
You may have had a vaccine against whooping cough before. This could have been when you were a child or during a previous pregnancy. The immunity you develop from being vaccinated wears off over time.
This means you’ll need to have the vaccine every time you’re pregnant. It’s the best way to protect your baby from getting ill from whooping cough.
If you have a new-born baby but were not immunised when pregnant
If you did not get your whooping cough vaccine when you were pregnant, speak to your midwife or health visitor. You may be offered the vaccine if your baby has not yet had their vaccinations at 8 weeks old.
About the whooping cough vaccine
Most people in Scotland will receive the ADACEL vaccine to help protect against whooping cough.
This vaccine protects against 3 different diseases:
- whooping cough (pertussis)
- diphtheria
- tetanus
There is no whooping cough only vaccine currently available.
If you cannot have the ADACEL whooping cough vaccine, an alternative vaccine (Boostrix-IPV or REPEVAX) may be suitable. Your midwife will be able to advise about which vaccine is right for you.
Read more about vaccine ingredients in the patient information leaflets:
The vaccine cannot cause whooping cough
The vaccine cannot cause whooping cough
The vaccine cannot cause whooping cough
The whooping cough vaccine is not a live vaccine. It cannot cause you or your baby to contract whooping cough. It’s the safest and most effective way to protect your baby from whooping cough.
You need 1 dose of the whooping cough vaccine
You only need 1 dose of the whooping cough vaccine for you and your baby to be fully protected. This is the same even if you’re expecting more than one baby.
You’ll need to get 1 dose of the whooping cough vaccine every time you’re pregnant.
The whooping cough vaccine protects
Getting the vaccine is an effective way of protecting you and your baby from whooping cough. A whooping cough vaccine has been offered in Scotland since 2012.
The vaccine offers around 90% protection against death from whooping cough in babies under 3 months of age.
Vaccine safety
All medicines (including vaccines) are tested for safety and effectiveness before they’re allowed to be used. Their safety continues to be monitored once in use. The vaccine meets the high safety standards required to be used in the UK and other European countries.
Respiratory Syncytial Virus (RSV) Vaccine
RSV vaccine during pregnancy
If you’re pregnant, you’ll be offered the RSV vaccine. It will help protect your baby against serious illness from RSV infection.
What the RSV vaccine is for
The respiratory syncytial virus (RSV) vaccine is offered during pregnancy. It helps protect your baby against serious illness caused by RSV infection.
RSV is a common respiratory virus. In most people it causes a mild illness with cold-like symptoms. It’s highly infectious and spreads easily when people with the virus cough or sneeze.
In Scotland, RSV is the most common reason that babies are admitted to hospital with respiratory (breathing) problems.
Those who are at highest risk of severe illness from RSV infection include:
- premature babies
- newborn babies (particularly in the first 6 months)
- children under 2 years with conditions that affect their heart, breathing or immune system
Older children and adults can also get infected with RSV. The disease is more serious for young babies.
RSV infection is more common in winter, but can happen at any time of year.
Who can get the RSV vaccine
You’ll be offered the RSV vaccine if you’re pregnant. It’ll help protect your baby against serious illness from RSV infection.
During pregnancy, you can get the RSV vaccine from 28 weeks. Having the RSV vaccine at this time means that your baby is protected even if they’re born early.
You should not get the RSV vaccine if you’re less than 28 weeks pregnant.
If you did not get the RSV vaccine at 28 weeks, you can still get it later in your pregnancy. It’ll still protect you from infection and reduce the risk of passing RSV infection to your newborn baby.
The best way to protect your baby from serious illness is getting all recommended vaccines at the right time.
Read more about the vaccines offered during pregnancy
About the RSV vaccine
The Abrysvo vaccine is offered in Scotland. It’s usually given as an injection in your upper arm.
The Abrysvo vaccine is not a live vaccine. It does not cause RSV infection.
There are very few people who cannot have the RSV vaccine.
You should not get the vaccine if you’ve had a severe allergic reaction (anaphylaxis) to:
- any of the vaccine ingredients
- a previous dose of the same vaccine
You can view the ingredients in the Abrysvo vaccine patient information leaflet.
It’s important to tell the person giving you the vaccine if you:
- have ever had a severe allergic reaction (anaphylaxis) to anything
- are receiving medicines, treatment or therapy at a hospital or specialist clinic
You need 1 dose of the RSV vaccine
You only need 1 dose of the RSV vaccine, even if you’re having multiple births (like twins or triplets).
If you get pregnant again in the future, you’ll need to get another dose of the vaccine at that time.
How the RSV Vaccine Works
The RSV vaccine boosts your immune system, which then produces more antibodies against the virus. These antibodies then pass through the placenta to your baby. This helps protect your baby from the day they are born.
The vaccine helps protect your baby
The vaccine has been shown to reduce the chance of your baby becoming very ill from RSV.
Like all medicines, no vaccine is 100% effective. If you have the vaccine, your baby may still get RSV. However, their RSV infection should be less severe.
If you get the RSV vaccine during pregnancy, the chance of your baby developing a serious infection caused by RSV reduces by over 80%.
The RSV vaccine has a good safety record
In a clinical trial of almost 4,000 women, the vaccine had a good safety record. It’s now been approved by medicines regulators in the UK, Europe and the USA. Many thousands of women have since had the vaccine in national programmes. This includes more than 100,000 women in the USA.
The clinical trial compared pregnant women who received the vaccine with those that had not. Slightly more babies were born early in the group that had the vaccine than in the group who had not had the vaccine. It’s thought that this difference is due to chance, and that there is not a link between vaccination and early birth. However, this is why the vaccine is being given from 28 weeks rather than earlier in your pregnancy.
Overall, it’s still safer for you and your baby to have the vaccine than to risk your baby getting an RSV infection.
All medicines (including vaccines) are tested for safety, quality and effectiveness before they’re allowed to be used. Once they’re in use, the safety of vaccines continues to be carefully monitored.
How to get the RSV vaccine
You should be offered the RSV vaccine around your 28 week antenatal appointment.
Speak to your midwife to find out the local arrangements for vaccination. They’ll be able to advise you on how to get your vaccine.
Flu Vaccine
Flu vaccine
Influenza (flu) is an infectious virus and can be serious. Symptoms may include a fever, a cough, a headache and tiredness. The virus spreads through the air when people cough or sneeze, or when they touch surfaces where the virus has landed then touch their eyes, nose or mouth. You can catch flu all year round, but it’s especially common in winter. It can be serious, even if you’re healthy.
The flu vaccine
The flu vaccine is the safest and most effective way to help protect against flu. It’ll also help reduce the risk of spreading flu to others.
The flu vaccine is available between September and March.
Why should I get vaccinated?
The flu vaccine has a good safety record. It gives the best protection against flu. It’s offered every year for free by the NHS to help protect people at risk of flu and its complications.
The vaccine helps protect against the main types of flu viruses. But there’s still a chance you might get flu after having the vaccine. If you do get flu, it’s likely to be milder and not last as long if you’ve received the flu vaccine.
Having the flu vaccine can also stop you spreading flu to other people who may be more at risk of complications and serious illness if they catch flu.
You have to get immunised every year because flu viruses change constantly and your immunity reduces over time.
The flu vaccine can’t give you flu, but it can stop you catching it.
Vaccine safety
All medicines (including vaccines) are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
Other Vaccinations
MPOX Vaccine
Vaccination to help protect against mpox (monkeypox)
Mpox (monkeypox) is a rare viral infection that usually causes a high temperature (fever) and a body rash that lasts a few weeks.
The risk of getting mpox in Scotland is low.
Who is offered the mpox vaccine?
The vaccine is recommended for people whose sexual networks mean they are more likely to come into contact with mpox. These include:
- gay, bisexual, men who have sex with men (GBMSM), those who have multiple partners, take part in group sex, attend sex on premises venues, or have had a bacterial STI such as chlamydia, gonorrhoea or syphilis in the past year
- some trans and non-binary people who are in similar sexual networks to GBMSM
- some healthcare workers in high-risk settings where they may care for a patient with mpox
How many doses will be offered?
A full course of 2 doses of vaccine given at least 28 days apart is recommended for those at risk of mpox exposure.
Where can I get the vaccine?
If you’re eligible, some specialist sexual health clinics are offering the MVA vaccine.
Find my nearest sexual health service
Healthcare workers at higher risk will be offered the vaccine from their employer.
The vaccine
Mpox is caused by a virus similar to the one that causes smallpox. So vaccines designed for smallpox are expected to prevent or reduce the severity of mpox.
The vaccine used in Scotland contains a virus that’s been modified so that it cannot grow in the human body. This Modified Vaccinia Ankara (MVA) vaccine is a much safer form of the smallpox vaccine. MVA vaccines do not contain smallpox virus and cannot spread or cause smallpox.
The MVA (Imvanex) vaccine has been authorised for immunisation against mpox as well as smallpox by the Medicines and Healthcare products Regulatory Agency (MHRA).
As there is no UK branded vaccine available, you may be offered the US labeled equivalent of the MVA (Imvanex) vaccine, which is called Jynneos. This is the same vaccine as Imvanex and is also approved for mpox.
Read the IMVANEX patient information leaflet
Read the JYNNEOS patient information leaflet
The vaccine helps the immune system (the body’s natural defence system) produce its own protection in the form of antibodies against the smallpox virus.
The UK Health Security Agency (UKHSA) and the Joint Committee on Vaccination and Immunisation (JCVI) recommend the MVA vaccine to help prevent mpox.
Vaccines are recommended to protect against disease. After vaccination, you should continue to be aware of the risks and symptoms of mpox.
How is the vaccine given?
Most vaccines are given by injection into the muscle of the upper arm (intramuscular) or the tissue just above it (subcutaneous).
Some vaccines can also be injected into the upper layer of the skin. This is known as intradermal vaccination. This is how the MVA vaccine to protect against mpox may be given.
Is the vaccine safe?
MVA vaccines meet the required standards of safety and effectiveness. Vaccine safety continues to be monitored once it’s in use.
Are there any reasons I can’t have the vaccine?
You should not have the vaccine if you’ve previously had a sudden life-threatening allergic reaction (anaphylaxis) to either:
- a previous dose of the MVA vaccine
- any ingredient of the vaccine, including those present in very small amounts such as chicken protein, benzonase, gentamicin or ciprofloxacin
It’s also important to tell the person giving you the vaccine if you:
- have a high temperature
- have atopic dermatitis (atopic eczema)
- are living with HIV or any other condition or treatment leading to a weakened immune system
- are pregnant, planning to have a baby or breastfeeding
You can also let them know if you:
- have a minor infection such as a cold
- are taking or have recently taken any other medicines
- have recently received any other vaccine
You can be given this vaccine even if you’ve received a smallpox vaccination in the past. But you may be at increased risk of side effects, so speak to the person giving you your vaccine.
Are there any side effects?
Like all medicines, the vaccine can cause side effects, but not everybody gets them. The common side effects are:
- a headache
- aching muscles
- nausea
- tiredness
- chills
- fever
- joint pain, pain in the extremities (hands and feet)
- loss of appetite
- pain, redness, swelling, hardness, itching, discolouration, a lump or bruising at the injection site
Around 1 in 10 people may have chills and fever, but these should not last more than a few days. If you experience any of these side effects, you should rest and take paracetamol. Always follow the manufacturer’s instructions. Do not take medicines containing aspirin if you’re under 16.
The most common side effects reported are at the site of injection. Most are mild to moderate in nature and cleared without any treatment within 7 days.
If you have atopic dermatitis (atopic eczema), you may experience:
- more intense skin reactions such as redness, swelling and itching
- other general symptoms such as headache, muscle pain, feeling sick or tired
- a flare-up or worsening of your skin condition
Can I pay for an MVA vaccine privately or at a pharmacy?
No, the MVA vaccination is only available through the NHS to eligible groups and it’s a free vaccination.
If you have been exposed to mpox
If you’ve had significant contact with someone with mpox, you may also be offered the vaccine. This includes healthcare workers in high-risk settings, who are caring for someone with confirmed mpox.
The vaccine is most effective when given within 4 days from the date of exposure. However, it can be given up to 14 days after exposure if you’re at high risk of ongoing exposure or at risk of more severe disease. This may reduce your symptoms but may not prevent disease.
Two doses are recommended for longer term protection against mpox. The second dose can be given at least 28 days after the first.
Are there side effects of the intradermal vaccination?
Common side effects after intradermal vaccination are:
- mild fever and tiredness
- moderate redness, swelling and itching at the injection site
Around a third of people who get the intradermal vaccination may develop a small dark mark at the injection site for some months.
This information is only a guide. If you’re concerned about any side effects, speak to your health professional or phone NHS 24 on 111 for free.
Student Vaccination
As your college or university term begins, remember to check your vaccines are up-to-date. Read about keeping yourself protected from serious diseases.
It’s really important for all students to ensure they’re up-to-date with their vaccines before starting college or university. You should have had:
Student Vaccination
Students in the NHS Greater Glasgow and Clyde are encouraged to ensure their vaccinations are up to date before returning to college or university this year.
Infectious diseases that can cause meningitis and other serious conditions can spread easily in universities and colleges. The Meningococcal ACWY (MenACWY) and MMR vaccines help to protect you against these very serious diseases, which is why it’s important to check that your vaccines are up to date.
Students are at higher risk of developing invasive meningococcal disease than the general population. The MenACWY vaccine helps protect against meningitis and septicaemia (blood poisoning). The vaccine is offered to young people because meningococcal disease is much more likely to spread within this group.
Meningitis and septicaemia are very serious, life-threatening conditions that get worse very quickly.
It’s also important to check that you’ve had two doses of the MMR vaccine. This protects against measles, mumps and rubella.
Measles can lead to serious and potentially life-threatening complications in some people. These include infections of the lungs (pneumonia) and brain (encephalitis).
There is also still time to get the human papillomavirus (HPV) vaccine, although most students will have received this at school. It helps protect against HPV-related cancers including head, neck and cervical cancer. It also protects against over 90% of genital wart infections.
What to do to if you’ve missed/to catch-up on vaccinations
- Glasgow University
- Strathclyde University
- Caledonian University
- University of the West of Scotland (Paisley Campus only)
If you are concerned about a missed vaccination, please discuss this with your GP and if appropriate, your GP will refer you for vaccination via SCI Gateway.
What vaccinations am I offered?
Students will be offered the following vaccines:
- MenACWY
- MMR
- Human papillomavirus (HPV)
If you require any other vaccines that are not listed above, please consult with your GP.
Student Vaccination Clinics
The next student vaccination clinics will be held at the following:
Strathclyde University – 18th September – 09:30 – 16:00
Human Papillomavirus (HPV) vaccine
Most students will have had the HPV vaccine at school. If you missed it, you may still be able to get it up until you turn 25.
This only applies to:
- people who are currently eligible
- boys who became eligible from the 2019/2020 academic year
- girls under 25 who were eligible under routine and catch up HPV vaccine programmes introduced in 2008
If you’re from Scotland and have not yet had the HPV vaccine, you first need to register with a GP practice local to your new address.
If you’ve come to Scotland from another country and know that you haven’t had the HPV vaccine, contact your local NHS immunisation team.
Read more about the HPV vaccine
The HPV vaccine is available in Scotland for men who have sex with men (MSM) up to and including 45 years old.
Men who have sex with men are offered the vaccine because they’re known to have a higher risk of HPV infection. The HPV vaccine may be offered to MSM at sexual health and HIV clinics across Scotland.
Read more about the HPV vaccine for men who have sex with men
If you don’t know what vaccinations you’ve had
If you’re not sure if you’re up to date on all your vaccines, you can check your red book to see immunisations you’ve had. If you don’t have a red book, contact your GP to check your vaccination records. If they cannot help, you can try contacting your local NHS immunisation team.
Students coming to Scotland from another country
Before you arrive in Scotland, you should check you’re fully up-to-date with vaccinations.
After you arrive, you may be eligible for free vaccines that are not available in your home country. Contact your local NHS immunisation team to get any vaccines you may have missed.
Read more about healthcare for those coming from overseas, and registering with a GP practice
Other Vaccinations
Was this helpful?
Flu and COVID-19 Vaccination
Flu and COVID-19 vaccines will be offered to those eligible between September and December. It’s strongly recommended you get vaccinated if you’re offered this winter. If you’re eligible, you’ll receive a letter, SMS or email with appointment details or information about how to book one. You may receive information about your appointment at a different time than previous years.
For more information about winter vaccines and who is eligible visit at NHS Inform.
Overview
We expect to offer a Flu and COVID vaccination (where eligible) to the eligible population across Greater Glasgow and Clyde, ranging from school aged children (flu only) to people living in care homes for the elderly.
The way you get your Flu and COVID vaccination will have changed over recent years. No Flu or Covid Vaccinations are delivered in General Practice. Vaccinations are given in a range of different settings:
Drop In Clinics
Drop in Vaccination Clinics
Winter vaccines Drop-in clinics
We’re encouraging those eligible to take up the offer of their flu and/or COVID-19 vaccines as soon as possible. Both viruses can be serious and evidence shows that COVID-19 vaccine protection fades and the flu virus changes over time. Getting vaccinated is the most effective way to protect yourself against serious illness.
If you’re eligible for vaccination and haven’t yet received one, or both, please come along to one of the drop-in clinics below to ensure you’re protected ahead of the festive season:
Community Clinic Drop-ins
Wednesday 31st December 2025
Renfrew North Parish Church: 14 Renfield St, Renfrew PA4 8RG -10:00-15:30
Saturday 3rd January 2026
Clydebank Health And Care Centre: Queens Quay Main Avenue, Clydebank G81 1BS – 10:00-19:00
Sunday 4th January 2026
Port Glasgow Health Centre: 2-4 Bay St, Port Glasgow PA14 5EW -10:00-19:00
Monday 5th January
Piazza: Unit-28/29, Central Way, Paisley PA11 ELB – 10:00-19:00
Tuesday 6th January
Piazza: Unit-28/29, Central Way, Paisley PA11 ELB – 10:00-19:00
Johnstone Town Hall: 25 Church St, Johnstone, PA5 8EG – 10:00-19:00
Wednesday 7th January
St Marks Church, 281 Kinfauns Drive, Drumchapel, Glasgow G15 7BD – 10:00-19:00
Thursday 8th January
Priesthill Community Hall, 100 Priesthill Road, Glasgow G53 6QL – 10:00-19:00
Milngavie Town Hall: 71 Station Rd, Milngavie, Glasgow G62 8BZ – 10:00-19:00
Broomhill Gardens and Community Hub, 46 Mearns St, Greenock PA15 4QD – 10:00-19:00
Friday 9th January
Renfrew North Parish Church: 14 Renfield St, Renfrew PA4 8RG -– 10:00-19:00
Saturday 10th January
Clydebank Health And Care Centre: Queens Quay Main Avenue, Clydebank G81 1BS – 10:00-19:00
Parkhead Hub, 1251 Duke Street, Parkhead, Glasgow, G31 5NZ – 10:00-19:00
Alexandria Community Centre: Main St, Alexandria, G83 0NU – 10:00-19:00
Mobile Vaccination Service
The Scottish Ambulance Mobile Vaccination vehicle is a drop in service. This means that there may be busy times and you may have to wait. The mobile clinic can only accommodate 4 vaccinators and a limited supply of vaccine. Please be patient. You may wish to book an appointment at one of our Vaccination Centres instead.
You can do this by going to the online booking portal or calling the National Contact Centre on 0800 030 8013.
The mobile vaccination service will offer Flu vaccinations on:
Tuesday 13th January 2026 – Craigend Resource Centre, McLeod Street, Greenock, PA15 2HD – 10:00am – 16:00pm
Wednesday 14th January 2026 – Thornliebank Health Centre, 20 Kennishhead Road, G46 8NY – 10:00am – 16:00pm
Thursday 15th January 2026 – Great Western Retail Park, 10 Allerdyce Road, G15 6RX – 10:00am – 16:00pm
Friday 16th January 2026 – Neilston Leisure Centre, Main Street, Neilston, G78 3NN – 10:00am – 16:00pm
Monday 26th January 2026 – Redbrae Road Car Park, 88a Redbrae Road, Kirkintilloch, G66 2DP – 10:00am – 16:00pm
Tuesday 27th January 2026 – Tweedie Hall (the car park beside Linwood health centre), 11 Bridge Street PA3 3DB – 10:00am – 16:00pm
Children and Young People
The vaccine will be offered to all school-aged pupils, all children aged 2-5 not yet in school and children aged 6 months to 2 years old with a condition that puts them at increased risk of flu. Home-educated young people and young people not attending mainstream education are also eligible.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu. Children aged 2 to 5 are being offered vaccination from September to ensure they receive the earliest protection and prevent the virus spreading.
Those eligible for the childhood and school flu vaccination programme include:
- Children aged from 6 months to 18 years in clinical risk groups (if not eligible in accordance with bullets below)
- All children aged 2-5 years not yet at school (age as of 01/09/2025)
- All primary school children (primary one to primary seven)
- All secondary school pupils (years one to six)
Winter Flu and COVID-19 Vaccination 2025
COVID-19 vaccinations will be offered to those who are eligible until 31st January 2026.
Flu vaccinations will be offered to those who are eligible until 31st March 2026.
Flu and Covid-19 vaccines will be offered to those eligible from October onwards. It’s strongly recommended you get vaccinated if you’re eligible this winter. Invitations for people who are eligible will start being sent from late August. You may receive your invitation at a different time than previous years. You should attend the appointment you’ve been given, or make or rearrange your appointment as soon as possible.
The postal invites will arrive in white envelopes with clear NHS Scotland branding. People with a digital preference will receive their vaccine appointment or prompt by text and/or email.
Please do not try to make an appointment until you’ve been invited by NHS Scotland.
The joint committee on vaccination and immunisation (JCVI) advice is to offer the vaccines to those at high risk of serious illness from flu or COVID-19 and who are therefore most likely to benefit from vaccination.
Who will be offered the flu vaccine
The flu vaccine is offered to adults who are most at risk of getting seriously ill from flu.
Older adults and people with certain health conditions are more at risk of flu-related complications and need extra protection, even if their health condition is mild or well managed.
You’ll be offered the flu vaccine this year if you’re:
- aged 65 and over
- aged 18 to 64 with an eligible health condition
- pregnant
- living in a long-stay residential care home or other long-stay care facility
- working in a care home for older adults
- living with someone who has a weakened immune system
- an unpaid or young carer
- a frontline health or social care worker
- a non-frontline NHS worker
- a poultry worker or bird handler
- an asylum seeker living in a home office hotel or B&B accommodation
- experiencing homelessness or substance misuse
- living in a Scottish prison
Who will be offered the COVID-19 Vaccine
Eligibility for the COVID-19 vaccination programme is based on the advice and recommendations of the Joint Committee on Vaccination and Immunisation (JCVI).
This is informed by robust evidence of which groups are at risk of severe disease, hospitalisation and death from COVID-19.
Vaccination will be offered to those at high risk of serious illness from COVID-19. These groups include:
- adults aged 75 years and over
- residents in a care home for older adults
- individuals aged 6 months and over who are immunosuppressed (as defined in the ‘immunosuppression’ sections of tables 3 or 4 in the COVID-19 chapter of the Green Book)
To find out if you are eligible for flu vaccination, please visit the Flu vaccine | NHS inform
To find out if you are eligible for COVID Vaccination please visit NHS Inform.
When will I be invited?
Please wait to be contacted about your vaccination – do not try to make an appointment until you’ve been invited by NHS Scotland.
NHSGGC Staff Only
Staff Vaccination 2025/26

Why act now?
Flu season has hit Scotland around a month earlier than usual, and cases are continuing to rise. NHSGGC is urging all staff to get their winter vaccinations now to avoid being floored by symptoms or, in severe cases, hospitalised.
There are multiple ways that staff can get the vaccine, listed below.
Participating community pharmacies
There is a list of around 180 pharmacies on the NHSGGC website that are offering the vaccine to eligible people. We recommend you contact them in advance to ensure they have a vaccinator ready when you pop in and remember to take your staff ID badge with you.
Pharmacies providing the vaccines can be found in the list below:
- Glasgow South
- Glasgow North East
- Glasgow North West
- Renfrewshire
- East Renfrewshire
- West Dunbartonshire
- East Dunbartonshire
- Inverclyde
Who is eligible?
- Health social care and social work staff who work directly with patients and provide support services are eligible for the flu vaccine this year.
- Non-frontline NHS staff are also eligible for the flu vaccine.
- Vaccination of staff groups will protect health services from staff absences during the winter months. It is recommended staff take up the offer of vaccination this year to protect those in their care and themselves.
To find out if you are eligible for flu vaccination, please visit the Flu vaccine | NHS inform
Winter vaccines for Health and Social Care Staff
Staff flu vaccinations – Staff Flu Vaccination Week is now complete. You can still receive your vaccination by:
For anyone that is hospital based, there are over 40 peer vaccinators working across our hospital sites continuing to offer staff vaccines within their ward settings.
Health and social care staff are also able to access community pharmacy to receive their flu vaccine at a time and place that is convenient to them. To find out participating pharmacies, please see ‘community pharmacy – Flu only’ section.
Community flu vaccination clinics are also available. These can be booked by visiting Login – Customer Service (nhs.scot) or calling 0800 030 8013 during the hours of Monday to Friday 9.00am to 6.00pm or Saturday 9.00am to 1.00pm.
For staff with a weakened immune system who access the national booking portal. They may say an automatic message advising them to wait until they have received their letter. This is directed at those staff members who are 65 or over, immunocompromised, or ‘at-risk’.
Your Appointment
About your Autumn/Winter Vaccination Appointment
- Where eligible Flu and COVID-19 vaccination will be given at the same appointment.
- Appointments will be available right the way through to December, ensuring all those eligible are protected before flu and COVID-19 viruses are most likely to be circulating.
- Most adults who are eligible for one or both vaccines will have already been contacted by NHS Scotland. Depending on communication preferences, this will have been by letter, email or text. Please attend the appointment you’ve been given, or make or rearrange your appointment as soon as possible.
- More information is available on Winter vaccines | NHS inform including a self-help guide that helps citizens to find out about the vaccines you may be eligible for, and how you’ll be offered them.
How do I reschedule my appointment?
You can rearrange your appointment if the time or day you’ve been given doesn’t suit you.
There may be evening and weekend vaccination clinics available too. If it’s more convenient, you can book or reschedule your appointment to a vaccination clinic closer to where you work or somewhere you visit regularly. This can be anywhere in Scotland.
If you are unable to attend or cannot get to this location, you can change your appointment online at:
Or you can call the helpline number to rearrange your appointment Monday to Friday 9.00am to 6.00pm on 0800 030 8013 or Saturday 9.00am to 1.00pm
Please note this number is for rescheduling appointments only.
Cancelling your appointment or opting out
NHS Scotland strongly recommends you get vaccinations when they are offered to you.
However, if you decide to cancel your appointment, you should do this online via the booking portal or phone the national vaccination helpline on 0800 030 8013. Appointments for children under 12 can only be cancelled by phoning the helpline.
If you wish to opt out, you will need to phone 0800 030 8013. You are only opting-out of coronavirus and flu vaccinations under the current programme. Please note that the way the IT system is built, you cannot opt out of one vaccine only. For example, if you are still interested in getting your flu vaccine, but not your coronavirus vaccine, you should not opt out. When offered a coronavirus vaccine at a future flu appointment, you can simply decline this.
If you previously opted out, this meant that we would no longer send you out a scheduled appointment for these vaccinations. You may have since received an invitation letter, text or email informing you of your eligibility for the winter vaccination programme, prompting you to book if you wish to do so. This is because NHS Scotland has a duty of care to inform you of the vaccines available to you. If you wish to opt out of all further communications about coronavirus and flu vaccinations, please call 0800 030 8013. If you are eligible for other vaccine programmes, you will still be invited for those. Your data will remain on the system, in case you wish to opt back in at any point in the future.
If you’re ill on the day
You no longer need to wait for a specific amount of time after confirmed Covid-19 infection to have your vaccine. However, if you’re unwell, wait until you’ve recovered to have your vaccine. You should not attend an appointment if you have a fever, diarrhoea or vomiting, or think you might be infectious to others.
What can I expect after my vaccine
Possible side effects of the flu vaccines
Like all medicines, the flu vaccine can cause side effects. This is normal but not everyone gets them. It shows the vaccine is teaching your body’s immune system how to protect itself from the disease.
These potential side effects are much less serious than flu or complications associated with flu.
Side effects are usually mild and may include:
- tenderness, swelling and/or redness at the site of the injection
- headache
- muscle aches
- fever (temperature 38°C or above)
You may also feel generally unwell. These possible side effects usually go away within a few days.
You can rest and take the normal dose of paracetamol (follow the advice in the packaging) to help make yourself feel better.
Possible side effects of the COVID-19 vaccine
Like all medicines, the COVID-19 vaccine can cause side effects. This is normal but not everyone gets them. It shows the vaccine is teaching your body’s immune system how to protect itself from the disease.
Side effects are usually mild and may include:
- a painful, heavy feeling and tenderness in the arm where you had your injection
- feeling tired
- headache
- general aches or mild flu-like symptoms
Side effects should normally only last a few days, and no longer than a week. Even if you’ve had side effects after a previous dose, it’s recommended you get all the doses you’re eligible for, unless your side effect was severe. If you have any questions, speak to your health professional or vaccinator. You can rest and take paracetamol (follow the dose advice in the packaging) to help make yourself feel better.
Where will I be required to attend for my appointment?
East Dunbartonshire
| Clinic | Facilities | Location/Transport |
| Milngavie Town Hall: 71 Station Rd, Milngavie, Glasgow G62 8BZ | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Milngavie Town Hall – Google Maps Bus – First Bus Train – ScotRail |
| Kirkintiloch Town Hall, Kirkintilloch, G66 1HN | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Kirkintilloch Town Hall Bus – First Bus Train – ScotRail |
Renfrewshire
| Clinic | Facilities | Location/Transport |
| Renfrew Parish Church Hall, 14 Renfield Street, Renfrew PA4 8RG | Parking Wheelchair Access Hearing Loop Toilet Facilities Interpreter Services | Renfrew Parish Church Hall Bus – First Bus Train – ScotRail |
| Johnstone Town Hall: 25 Church St, Johnstone, PA5 8EG | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Johnstone Town Hall – Google Maps Bus – First Bus Train – ScotRail |
| Piazza Shopping Centre Unit-28/29, Central Way, Paisley PA1 1ELB | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Piazza Shopping Centre Bus – First Bus Train – ScotRail After 6pm, please use the Smithhills Street entrance to the Piazza Shopping Centre |
East Renfrewshire
| Clinic | Facilities | Location/Transport |
| Eastwood Health Centre, Drumby Cres, Clarkston, Glasgow G76 7HN | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Eastwood Health Centre Bus – First Bus Train – ScotRail |
| Barrhead Health & Social Care Centre, 213 Main St, Barrhead, Glasgow G78 1SA | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Barrhead Health & Care Centre – Google Maps Bus – First Bus Train – ScotRail |
Glasgow City
| Clinic | Facilities | Location/Transport |
| Stobhill Hospital Seminar Rooms, car park 3 entrance, 133 Balornock Road, Glasgow G21 3UW | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Stobhill Hospital Bus – First Bus Train – ScotRail The clinic is situated at the rear of Stobhill Hospital (Seminar Rooms) Go through main entrance door and continue to the exit directly at the rear of the building. The seminar rooms are at the building on the left. |
| Gorbals Health & Care Centre, 2 Sandiefield road, Gorbals, G5 9AB | Parking Wheelchair access Hearing Loop Toilet Facilities | Gorbals Health & Care Centre |
| Institute of Neurological Sciences, Queen Elizabeth 1345 Govan Road, Glasgow G51 4TF | Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Institute of Neurological Sciences Bus – First Bus Train – ScotRail |
| Parkhead Hub, 1251 Duke Street, Parkhead, Glasgow, G31 5NZ | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | The Parkhead Hub Bus – First Bus Train – ScotRail |
| Priesthill Community Hall, 100 Priesthill Road, Glasgow G53 6QL | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Priesthill Community Hall Bus – First Bus Train – ScotRail |
| St Marks Church, 281 Kinfauns Drive, Drumchapel, Glasgow G15 7BD | Hearing Loop Toilet Facilities Baby Changing Interpreter Services | St Mark’s Church – Google Maps Bus – First Bus Train – ScotRail |
| Greater Easterhouse Supporting Hands, 1 Redcastle Sq, Glasgow G33 5EG | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Greater Easterhouse Supporting Hands – Google Maps Bus – First Bus Train – ScotRail |
| Whiteinch Centre, 1 Northinch St, Glasgow G14 0UG | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Whiteinch Centre Bus – First Bus Train – ScotRail |
| Castlemilk Health Centre, 71 Dougrie Drive, Glasgow, G45 9AW | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Castlemilk Health Centre Bus – First Bus Train – ScotRail |
West Dunbartonshire
| Clinic | Facilities | Location/Transport |
| Alexandria Community Centre: Main St, Alexandria, G83 0NU | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Alexandria Community Centre – Google Maps Bus – First Bus Train – ScotRail |
| Concorde Community Centre, St Mary’s Way, Dumbarton G82 1LJ | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Concorde Community Centre – Google Maps Bus – First Bus Train – ScotRail |
| Clydebank Health And Care Centre, Queens Quay Main Avenue, Clydebank G81 1BS | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Clydebank Health And Care Centre Bus – First Bus Train – ScotRail |
Inverclyde
| Clinic | Facilities | Location/Transport |
| Port Glasgow Health Centre, 2-4 Bay St, Port Glasgow PA14 5EW | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Port Glasgow Health Centre Bus – First Bus Train – ScotRail |
| Broomhill Gardens and Community Hub, 46 Mearns St, Greenock PA15 4QD | Parking Wheelchair Access Hearing Loop Toilet Facilities Baby Changing Interpreter Services | Broomhill Gardens and Community Hub Bus – First Bus Train – ScotRail |
Community Pharmacy – Flu Only
You’ll be offered the flu vaccine this year at our participating pharmacies if you’re:
- aged 65 and over
- aged 18 to 64 with an eligible health condition
- living in a long-stay residential care home or other long-stay care facility
- working in a care home for older adults
- living with someone who has a weakened immune system
- an unpaid or young carer
- a frontline health or social care worker
- a non-frontline NHS worker
- a poultry worker or bird handler
- an asylum seeker living in a home office hotel or B&B accommodation
- experiencing homelessness or substance misuse
Participating Pharmacies:
Adults aged 16-18yrs who remain in secondary education will not be vaccinated in community pharmacy. This cohort will be picked up by the School Health Service. If your child has missed their vaccination in school,(i.e. due to sickness) the chilhood vaccination team will revisit the school and arrange for your child to be vaccinated. Childhood flu vaccination are not available in community pharmacy.