(Formerly Computerised Cognitive Behavioural Therapy, cCBT)
Welcome to Digital Therapies
Our Team of Clinical Psychologists, Administrators and Assistant Psychologists cover all of NHSGGC which includes all 6 HSCPs: – Glasgow; East Dunbartonshire; West Dunbartonshire; Renfrewshire; East Renfrewshire; Inverclyde.
Our range of Digital Interventions offer support for those experiencing mild to moderate Mental Health conditions
We have a series of both supported and un-supported Digital Therapy programmes.
For further information, our Team can be contacted via email at ggc.DTT@nhs.scot or by telephone to 0141 287 0295 Monday to Friday: – 9am to 4.30pm
We average approximately 50 daily referrals and aim to process all inbound referrals within 5 working days of receipt for our referred Supported SilverCloud programmes.
Digital Therapy – What to expect
- Structured Modules – Most of the programs are organised into structured modules, each addressing specific aspects of the user’s difficulty.
- Interactive Exercises – Users engage in interactive exercises and self-assessment tools to build skills and track progress.
- Support and Feedback – For our supported programmes a member of our Team will provide support and feedback during a set time period.
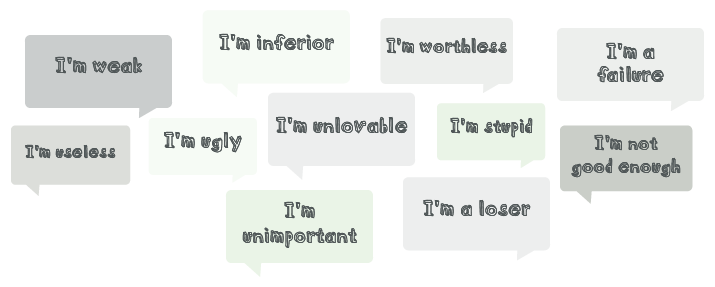
- Evidence-based techniques – Our Digital Therapies programmes use a Cognitive Behavioural Therapy (CBT) approach, this employs proven techniques like cognitive restructuring, exposure therapy and behavioural activation.
- Progress tracking – Users can track their progress and monitor improvements in their mental well-being over time
Digital Therapy – Free Access – No wait times
- When you’re struggling with your mental health, every day can feel like a challenge.
- Some days are good, but on others, even small daily tasks seem overwhelming.
- Perhaps you feel out of control, constantly worried, or like you are carrying around a weight that no-one else can see.
- In fact, most patients showed improvements in just three months.
- We’d love to get you started as soon as possible, please speak with your GP or dedicated Health care Specialist
- The programmes are available at any time of day and from any device, including a tablet or your mobile phone.
- And because every person’s situation is unique, each programme can be personalised.
- Contact your GP/Health Care Professional and ask for a referral to NHSGGC Digital Therapy for SilverCloud, or you can access our Self-Help programmes.
Long Term Conditions – Digital Interventions
Information on Digital Interventions for Long Term Conditions can be found by clicking on the buttons below.
Digital Therapy – Self Help Programmes
We have a range of Self-Help programmes for you to choose from.
These vary from help with anxiety and disturbed sleep patterns, to stress, resilience and Mental Health and Wellbeing.
You do not need a referral from your GP/Health Care Professional to access any of these self-help programmes.
Self-Referral Digital Therapy Interventions (Un-Supported)
- Space from Stress
- Space for Resilience
- Space for Positive Body Image
- Space from Money Worries
- Supporting an Anxious Child
- Supporting an Anxious Teen
https://wellbeing.silvercloudhealth.com/signup (Access code: ‘Scotland2020’)
Sleepio – is an NHS recommended digital treatment, which uses Cognitive Behavioural Therapy (CBT) to address poor sleep and insomnia and is free to everyone aged 18+ across Scotland. Click on Get Started. Complete the questionnaire then follow the instructions to set up your account.
Daylight – is a fully automated digital worry and anxiety improvement program based on techniques from cognitive behavioral therapy (CBT) for worry and anxiety. Click on Get Started. Complete the questionnaire then follow the instructions to set up your account.
More information on Sleepio and Daylight can be found at Big Health
Who can refer to Digital Therapies
- GPs (via SCI Gateway) and Clinicians within NHS who have an agreed secondary care pathway with the Digital Therapies Team
- We would recommend viewing our videos (to be uploaded in the near future) for further information, these have been prepared to offer guidance to ensure suitable referral to our Digital Therapies Team.
Mental Health Conditions – Digital Interventions
Digital Therapy for Mental Health Conditions
We offer a range of dedicated Digital Therapy Interventions for patients suffering from mild to moderate Mental Health Issues.
These range from Anxiety; Depression to Health or Social Anxiety; OCD; Panic or Phobia.