What assessments and tests will I have before treatment?
The nurse or doctor at your initial clinic consultation will advise which investigations and tests you need before starting treatment. See Screening tests and Initial Appointments – NHSGGC for a list of common tests and investigations.
Can I decline any investigations or tests?
You can always refuse any investigations or treatments. However, this may limit the advice or treatment we can offer.
What should I be doing while trying to conceive or preparing for fertility treatment?
There are lifestyle changes you and your partner can benefit from at this stage. Visit Lifestyle Advice – NHSGGC for more information. While preparing for your first appointments contact your GP to ensure your smear is up to date, you’ve had 2 MMRs and your partner’s semen analysis is in date.
If you don’t have 2 MMR vaccinations you can visit General Vaccinations – NHSGGC for information on MMR drop-in clinics.
You may also find these websites helpful for further advice Useful Links – NHSGGC
I have been told I’m on the waiting list, what happens next?
There are different waiting lists for each treatment. Once you have reached the top of the waiting list you will receive a letter inviting you to your first appointment with the nurses. While you’re waiting see Lifestyle Advice – NHSGGC
How can I see HFEA and patient ratings for the clinic?
We are regularly inspected by the HFEA and ask patients to submit feedback via their website. See HFEA: UK fertility regulator for recent inspections and patient ratings.
Can I use weight loss injections while having fertility treatment?
No. There isn’t enough evidence to show these drugs are safe in pregnancy. Some studies in animals have shown they are toxic to the developing foetus (baby). Please let your nurse or doctor in the clinic know if you are taking weight loss injections. See GLP-1 medicines for weight loss and diabetes: what you need to know – GOV.UK for more information.
Will I be able to book a treatment cycle when I want?
Once you have been told you can start treatment you can phone the booking line with your next period. However, we may not have a treatment cycle (slot) available for you to start. This is because we need to safely and effectively manage the number of patients having treatment at the same time.
When you phone the booking line to book a cycle they will be able to tell you if you have a slot or whether to call back next month. Sometimes it can take around 3 months to start treatment, particularly if you are planning a frozen embryo transfer cycle.
I don’t have a record of 2 MMRs, what can I do?
There are 3 ways to book MMR vaccinations.
- See your GP
- Visit General Vaccinations – NHSGGC for information on MMR drop-in clinics
- The ACS medics can refer you to a vaccination clinic once you have reached the top of the waiting list. Ask a nurse at your ART appointment.
I’ve been sent vaginal swabs to do, how do I do them?
Before you collect the sample, you can take the sample at any time of the day.
1. Wash your hands using soap and warm water, rinse and dry.
2. Open the swab packet where it says ‘peel here’.
3. Remove the swab container from the packet, (leave the swab INSIDE the packet at this stage) and label the container with your name, date of birth and the date and time the sample is being taken.
4. Twist the cap on the container tube to break the seal. Do not use if the seal is broken or damaged. Pull the cap off the container tube. Rest the container so the open end is uppermost, and the edges are not touching anything (it is a good idea to stand it upright in a clean mug).
5. Remove the swab from the packet. Touch only the blue top. Do not touch the white stalk or soft tip, or lie the swab down. If you touch or drop the swab tip or the swab is laid down, discard the swab.
6. Stand or lie in a comfortable position (as you would when inserting a tampon, for example). Hold the swab by the blue cap with one hand so the swab tip is pointing toward you. With your other hand, gently spread the skin outside the vagina. Insert the tip of the swab into the vaginal opening. Point the tip toward your lower back and relax your muscles.
7. Gently slide the swab no more than two inches into the vagina. If the swab does not slide easily, gently rotate the swab as you push. If it is still difficult, do not attempt to continue. Make sure the swab touches the walls of the vagina so that moisture is absorbed by the swab.
8. Rotate the swab for 10 to 15 seconds. Withdraw the swab without touching the skin. Place the swab in the container tube and push the cap in securely.
During Treatment
Should I contact you if I have a period after my Prostap injection?
A period after prostap is expected and you don’t need to contact us. It is normal after prostap to have a slightly longer, heavier or more painful period.
Should I contact you if I do not have a period after my Prostap injection?
No, attend your next appointment as arranged and you will have an ultrasound scan and blood test to check your hormone levels. You may need further medication prescribed.
What side effects should I expect during treatment?
Common symptoms include: Tiredness, Nausea (feeling sick), Vomiting (being sick), Diarrhoea, Weight gain and Pain or swelling of the stomach. You may also notice redness, bruising, swelling and/or itching at the injection site.
In cases of severe OHSS you may have: Fluid build-up in the stomach, pelvis and/or chest, Difficulty in breathing, Decreased urination (producing less urine when you go to the toilet or going to the toilet less often), Formation of blood clots in blood vessels (thromboembolism) or Twisting of ovaries (ovarian torsion). If you notice any of the above signs, contact the clinic immediately. Ovarian hyperstimulation syndrome (OHSS) | RCOG
I have dropped/smashed/wasted some of my medication, what should I do?
If you have enough medication to last until the next appointment, keep taking it as instructed and we will give you more at the next appointment.
If you do not have enough, please contact the nurses before 6 pm.
If it is after 6pm and you need to take the medication that night please phone Ward 56 GRI (0141 211 4433) and ask if they have a supply of the medication. Please have the name & dose of the drug prescribed. Please note, the ward do not store every medication and this option should only be used in an emergency.
If I miss a dose of medication, what do I do?
Take a dose as soon as you remember, then continue as instructed.
Can I continue to have intercourse?
We advise you not to have unprotected intercourse during treatment to avoid the risk of a natural pregnancy, either while taking medication, after egg collection or after embryo transfer.
Male partners should leave 2 days since their last ejaculation when providing a sample of sperm for treatment.
After embryo transfer, it is recommended that you avoid intercourse for 3 days.
Can I fly?
Yes, there is no evidence that flying affects any aspect of your treatment.
While having treatment you should be available to attend appointments as needed.
Travel may have impact on treatment as certain areas are at risk of infection, such as zika and ebola disease. This may mean a delay to treatment as there can be serious consequences to pregnancy.
If travelling abroad, please refer to the Welcome to JPAC website for information on which countries are affected by zika and ebola disease.
Can I have dental treatment?
You should inform your dentist you are having fertility treatment and they will advise you accordingly
Can I colour my hair?
Yes, there is no evidence that colouring your hair affects any aspect of your treatment.
After Treatment
Is bed rest recommended following embryo transfer?
No, there is no evidence to suggest that bed rest following embryo transfer improves pregnancy rates. There is some evidence to show bed rest can reduce pregnancy rates.
Can I fly?
Yes, there is no evidence that flying affects pregnancy rates following embryo transfer.
Can I have dental treatment?
You should inform your dentist you may be pregnant and they will advise accordingly.
Can I colour my hair?
Yes, there is no evidence colouring your hair affects pregnancy rates following embryo transfer.
If I bleed before my pregnancy test should I contact the department?
No, continue with the medication you have been prescribed and perform your pregnancy test on the recommended date. If you have a positive test and are bleeding, then contact the department as we may wish to assess you further.
If I experience any symptoms of Ovarian Hyperstimulation syndrome should I seek medical assistance?
Yes, if you have any symptoms of OHSS you should contact the department and we will provide you with advice or arrange for you to attend the department for assessment by one of our doctors.
If I have had a positive pregnancy test do I continue on my medication?
Follow the advice on the letter given to you at your embryo transfer / IUI. If you had a fresh embryo transfer you do not need to continue on any medication, unless prescribed by a consultant.
If you have had a frozen embryo transfer you should refer to your protocol for advise on which medication should be continued. To arrange a further supply:
NHS patients – contact the nurses
GRFC patients – contact the admin team 0141 956 0509 option 4
If you were having IUI and were on buserelin injections you should stop.
I have had a positive pregnancy test but have had some bleeding/spotting/discharge, what should I do?
If the bleeding is not heavy, please contact the nurses and a nurse will contact you on or before the next working day. However, if the bleeding becomes heavier or you start to feel unwell, attend your nearest Accident and Emergency (A&E) department.
Can I request copies of my notes?
Yes, you can ask for copies of your clinical notes. Please visit Access to Records – NHSGGC for more information on how to make a request.
Please note, clinic staff are not allowed to provide patients with copies of their notes.
Laboratory FAQs
Semen Analysis
What will a semen analysis test tell me about the quality of my sperm?
A semen analysis is carried out to estimate the number of sperm, their movement (motility) and shape (morphology) in a sample.
When will I get the results from my semen analysis?
A doctor or nurse will explain the results at your next clinic appointment. Unfortunately, we cannot give you these results over the telephone.
Where do I produce my semen sample?
We have dedicated rooms on-site for sample production. We recommend semen samples to be produced on-site, however if you are unable to use our rooms you may produce at home as long as you can get the sample to the ACS within 60 minutes. You must use a sample pot provided by the ACS.
Sperm Freeze
I won’t be available on the day of my partner’s IUI /egg collection. How can I provide a sperm sample for treatment?
If your occupation (i.e. Armed forces, offshore working) means you will not be available to provide a fresh sample of sperm for treatment, you may be able to freeze sperm for back-up. You would need to attend an appointment for blood tests and consents to be taken, and then make a second appointment before the treatment day to ensure we can freeze a sperm sample to use on the day of treatment.
If you are available on the day of egg collection or IUI, a fresh sample is always preferred.
Sperm Preparation
What does “sperm washing” mean?
Before the sperm is used for treatment, the sample is washed to separate the sperm from the ejaculate. The washing procedure can also help to isolate the sperm with more movement.
IUI (Intrauterine Insemination)
What can I expect from an IUI procedure?
The procedure is very similar to a smear test. A speculum is inserted into the vagina in order to pass a catheter through the cervix. Attached to the catheter is a syringe containing prepared (‘washed’) sperm. When the catheter is in the correct position, the operator will depress the syringe and the sperm will be deposited into the uterus. The catheter is very fine and is normally not felt by the patient.
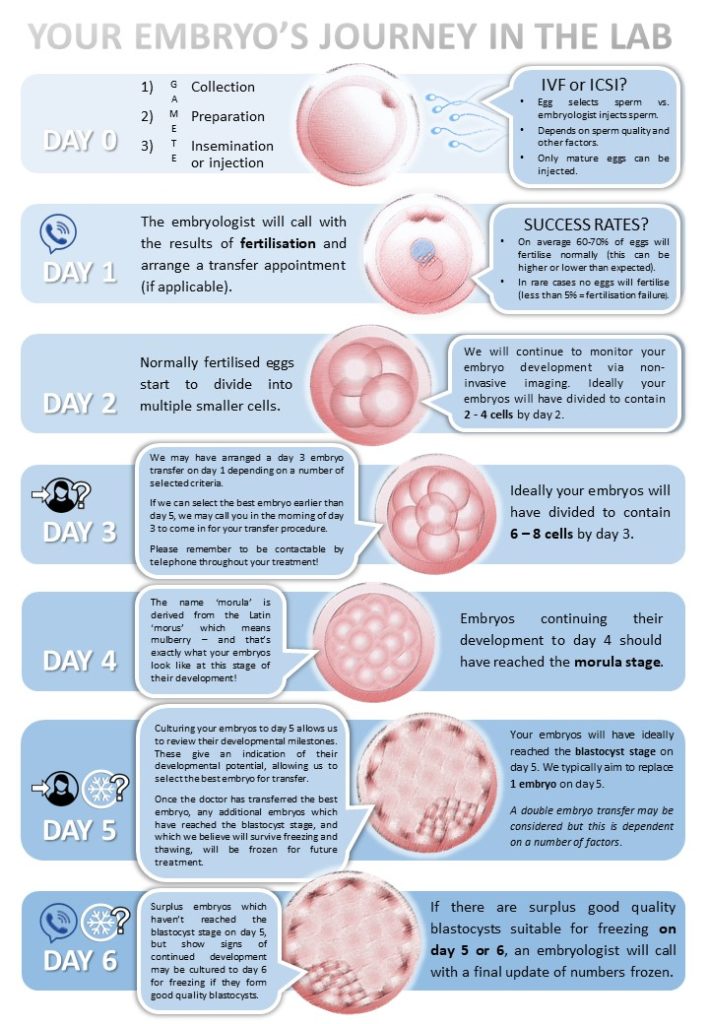
Embryology Laboratory Timeline for IVF and ICSI
Below is a general overview of the laboratory work and what can be expected at each stage of the journey
Oocyte retrieval
What preparation do I need for egg collection?
The nurse will give you a list of instructions to prepare for egg collection once the date of the procedure is known. They will give you an exact date and time to administer the booster injection.
You should fast from midnight before the egg collection, which means no food or fluids, including water.
On the day of egg collection, you should shower in the morning but not use any scented or perfumed products. If your partner is attending to provide a sample of sperm, they should do the same.
Bring any leftover medication and sharps boxes for disposal.
The anaesthetist requests that at least one fingernail be free from gel, acrylics or nail varnish.
Will I find out how many eggs were collected on the day of treatment?
Yes, the doctor performing your egg collection will meet with you after the procedure to discuss the number of eggs that were collected.
Can my partner stay with me during egg collection and recovery?
Partners are not permitted in theatre during the egg collection.
Due to the limited space in recovery, partners cannot stay with you during recovery.
IVF (In Vitro Fertilisation)
What is IVF?
IVF involves the collection of eggs directly from the ovaries using a needle. Washed sperm are added to a dish containing the eggs and the sperm are left to swim to the eggs on their own. The ‘best’ sperm that reaches the egg first should hopefully enter the egg and fertilise it.
The sperm and eggs are left in the dish together overnight and the eggs checked for fertilisation the following morning.
ICSI (Intracytoplasmic sperm injection)
What is ICSI?
ICSI involves the collection of eggs directly from the ovaries using a needle, then the injection of a single sperm into each mature egg to create embryos. ICSI is often recommended to patients if the sperm quality is not high enough to fertilise your eggs using IVF. ICSI can also be recommended to patients with previously low or complete failure of fertilisation in previous treatment.
I have a normal sperm count, why is ICSI still recommended for our treatment?
For some patients, ICSI is recommended even if sperm parameters are normal. The doctor or nurse will provide you with more information during a clinic appointment. Even when the planned treatment is IVF, this may change on the day of egg retrieval depending on sperm quality and number of eggs collected.
If you wish you can discuss this with your clinician and our embryology team.
Why aren’t all of my eggs suitable for IVF/ ICSI?
Only mature eggs have the capacity to fertilise, so before an ICSI procedure, your eggs will be assessed for maturity. Only the mature eggs will be used for ICSI.
Fertilisation Check
How many of my eggs should I expect to fertilise?
Our average fertilisation rate with ICSI is around 70%.
Some people may have a higher fertilisation rate and some people may have a lower rate.
When will I find out how many of my eggs have fertilised?
The embryologist will carry out a fertilisation check on your eggs the morning after your egg collection. You will receive a call on the same morning and the embryologist will inform you of your fertilisation results. You should expect the call to be before 12 noon.
Embryo Grading
What is a blastocyst?
A blastocyst is an embryo that has usually formed by day 5 or 6 after fertilisation and has two distinct cell types. The inner cell mass will develop into a baby, and the trophectoderm cells develop into the placenta.
How will you assess my embryos?
Embryo grading is carried out on day 3 and day 5 after your egg collection. On day 3 the embryologist will count the cell numbers and will take into account any fragmentation and unevenness of the cells. On day 5 blastocysts are graded by how expanded they are and the appearance of two cell types, the inner cell mass and the trophectoderm.
We are currently developing information leaflets to help us describe your embryo development in more detail. These should be available in the ACS waiting room and the consultation rooms in the very near future.
Embryo Transfer
What should I expect during an embryo transfer procedure?
The embryo transfer is very similar to a smear test. A speculum is inserted into the vagina and an empty catheter is passed through the cervix. Once the empty catheter is in position, a catheter containing the embryo is passed through the empty catheter and the embryo is deposited from the catheter into the uterus. The catheter is very fine and is normally not felt by the patient.
An abdominal (tummy) scan is used for guidance during the embryo transfer procedure. To ensure the best possible view, we ask that you have a comfortably full bladder in preparation for embryo transfer.
What is the difference between a day 3 or day 5 transfer?
Transfer days are based upon assessment of your embryo/s in the laboratory, which occur on day 3 and day 5. If a group of embryos on day 3 has a similar appearance and embryo selection for transfer cannot be made, a day 5 transfer will be arranged for you. If the embryologists think a transfer on day 3 is better for you, they will arrange this.
Can I take a picture or video during embryo transfer?
As advised by NHS GG&C policy, we do not allow any photography or filming in any areas of the ACS to protect the privacy of patients, staff and visitors.
Embryo Freezing (vitrification)
I didn’t have any embryos frozen. What does this mean?
For an embryo to survive the freezing and thawing process, it must be at the correct stage of development and be of suitable quality. The highest grade of embryo will be selected for transfer and if any surplus embryo/s meet our criteria we will freeze (vitrify) and store those embryo/s for you.
Some embryos may not reach the correct stage of development, or they may not meet the quality criteria, which is why we are unable to freeze them.
The doctor or nurse will meet with you before transfer to discuss embryo quality and let you know if any embryos are suitable to be frozen.
When will I find out how many embryos I have frozen?
The embryologist will phone the day after embryo transfer to confirm if we have been able to freeze embryos for you.
Frozen Embryo Transfer (warm/thaw)
How many embryos are likely to survive the freezing and thawing procedures?
Currently, our average survival rate for day 5 embryos is more than 95%.
Embryo Biopsies
Why are biopsies performed?
Biopsies are carried out for patients having a certain type of treatment called Pre-Implantation Genetic Testing (PGT). Most patients will not have embryos biopsied.
When are embryos biopsied?
Biopsies are performed on day 5 or 6 of blastocyst embryo development. Embryos are then frozen here in ACS and the biopsied cells are transported to the appropriate genetic lab.
How will I get the results?
An embryologist will call you with the results of genetic testing and explain the next steps.
General
Is there a set timeframe for the clinic to reply when you leave a message?
The clinic staff carry out procedures or see patients in appointments throughout the day; however, we endeavour to reply to all queries until 6pm. Messages after 6pm will be responded to the following day.
Before emailing, please check to see if your question can be answered here first.
What number should I be calling to enquire about treatment/appointments?
GRFC patients should call 0141 956 0509 option 4 for treatment bookings and appointment enquiries
NHS patients:
- For treatment bookings, please call 0141 201 3478
- For appointment enquiries, please call reception on 0141 211 8535
What is the current wait times from referral to starting first cycle?
Current waiting times are approximately 10 to 11 months.
How long after finishing a treatment cycle will I wait till I start a new fresh cycle or FET transfer?
If you have had a negative outcome or freeze all and are eligible for further treatment, you can phone with your first normal period to book your next cycle. If you do not have regular periods, you can call 4 weeks after your withdrawal bleed.
Whilst we try to accommodate all bookings, there are times when the numbers of attempted bookings exceed our capacity. In such cases, we advise patients to call with their next period. It may take around 3 months to be able to book a cycle.
When I phone to book a frozen embryo cycle or IUI, how long should I wait to hear if I have a slot?
Although we try to allocate slots daily, it can take up to a week before we can contact you to advise if you have a treatment slot, or not.
If it takes 7 days for a reply, does it mean I need to wait for my next cycle?
Not always. You may have a slot booked and will still have time to attend the necessary appointments.
Can I still do vaginal swabs when having my period?
Yes, please do the swabs as requested before your appointment.
Can I have a scan while on my period?
Yes, sometimes it is necessary to perform a scan at the start of a period, so please don’t worry about attending for a scan at this time.
I need to book a scan on a specific day of my cycle, how do I do this?
Contact the ACS nurses. Contact details can be found on your treatment card.
I’m having IUI or natural FET treatment and have detected a surge.
Call reception on 0141 211 8535 and they will book a blood test for you that morning.
I need more medication.
NHS patients – contact the nurses
GRFC patients – contact admin on 0141 956 0509 option 4
What is the best home ovulation test or pregnancy test to use?
We are unable to recommend specific tests but individual product information will be able to advise on sensitivities.
My case was being reviewed but I haven’t been notified of the outcome.
Every week all treatment cycles which have recently been completed are reviewed by the medics and embryologists. You will receive a letter summarising the outcome of the review meeting and your next steps.
Do I need to come to the clinic for my medication or can it be collected at my local pharmacy?
Most medication dispensed in ACS is very specialised and will not be available in every pharmacy. However, some common medications such as antibiotics may be available to be prescribed locally.
Accordion title 1
This is a placeholder tab content. It is important to have the necessary information in the block, but at this stage, it is just a placeholder to help you visualise how the content is displayed. Feel free to edit this with your actual content.
Accordion title 2
This is a placeholder tab content. It is important to have the necessary information in the block, but at this stage, it is just a placeholder to help you visualise how the content is displayed. Feel free to edit this with your actual content.