Recent previous winners of our Excellence Awards, Local Staff Awards, Chair’s Awards of Excellence, and the William Cullen Prize.
2024

2023

2021/2022
2019

2018

2017

2016

Recent previous winners of our Excellence Awards, Local Staff Awards, Chair’s Awards of Excellence, and the William Cullen Prize.






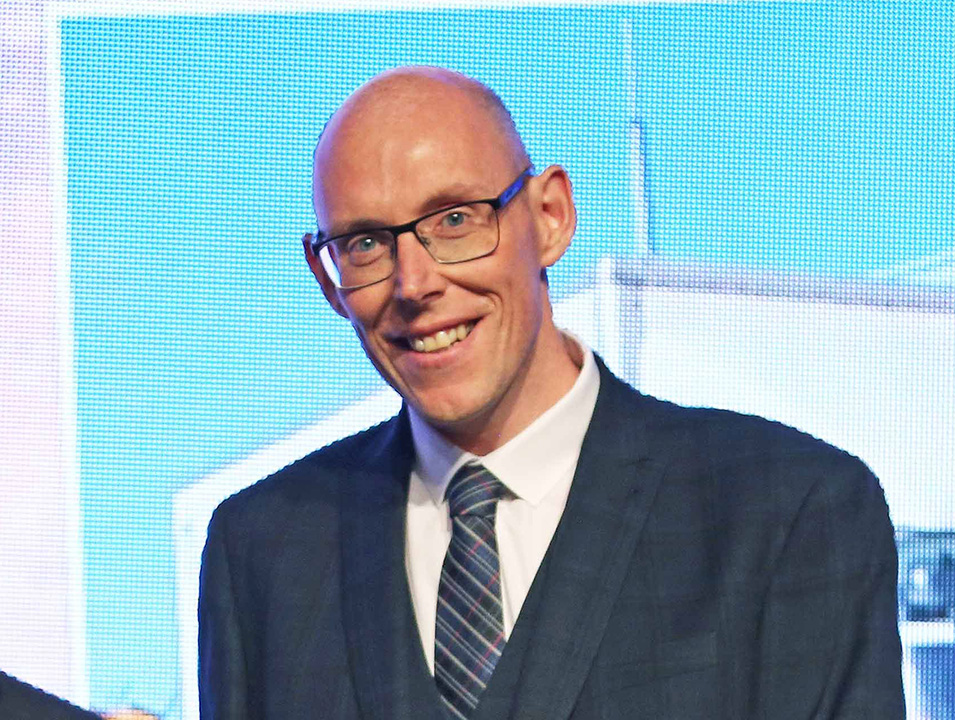
This year the Chair, Prof John Brown CBE, presented two awards which recognise outstanding achievement, expertise, and dedication in patient care. In common with all the other awards, these celebrate our people’s collective efforts and the lasting impact they have had on the lives of the people of Greater Glasgow and Clyde.
One of Andrew’s patients was going through a high risk pregnancy, when her husband sadly passed away after a two week battle with cancer. On hearing the news, Andrew called to offer his condolences and also talk about how he and his team could support the patient during this heart breaking time.
Andrew has an incredible way of communicating with patients and their families, with empathy and intuitiveness in abundance.
Due to unprecedented pressures, our Urgent and Unscheduled Care services have adapted to new and ever-changing situations which have been nothing short of remarkable. From the launch of the Flow Navigation Centre and Mental Health Assessment Units, to the ongoing dedication, commitment and professionalism of our EDs, IAUs, Community Pharmacies, MIUs, in-hours and Out of Hours GP Services, who have worked tirelessly with the support of diagnostic services.
At the start of the pandemic, it became clear that those who became very ill with Covid need a place where they could be seen and assessed safely and away from non-Covid patients.
Our Community Assessment Centres were created. This significant project required input from all of the eHealth teams to ensure the centres had all the necessary telephony and IT kit. They also needed to be set up very quickly.
eHealth teams responded to the needs of the service, working above and beyond to introduce new processes to book in Covid patients outwith hospital settings. The staff showed immense flexibility and changed their hours of work and their roles. The success of the CACs was due to the commitment, flexibility and team working across eHealth to support the Board in its response to the pandemic.
The William Cullen Prize for Excellence In Teaching and the William Cullen Prize for Service Innovation are awarded in collaboration with the Royal College of Physicians in Edinburgh.
Dr David Lockington is a Consultant Ophthalmologist based in Gartnavel General Hospital.
Dr Lockington identified the opportunity to transform unused rooms within the Tennent Institute of Ophthalmology library into a state of the art teaching suite for ophthalmology training. There are now three rooms which consist of an ophthalmic simulation area, a computer room for trainees and a seminar room.
The suite allowed simulated microsurgical skills to be developed and maintained during lockdowns, and is now used regularly by trainees and the wider multidisciplinary team. This development has been extremely well received by local trainees, and has addressed previously identified surgical training gaps.
Local ophthalmology training has been enhanced significantly, and to illustrate the impact, this initiative has since been replicated in other UK centres.
Doctor Scott Morris is the Clinical Director for the Renal Unit, based in the Queen Elizabeth University Hospital, though which provides a full range of renal services to the West of Scotland.
This unit has for some time demonstrated a high standard of teaching and training, as evidenced by consistent and positive feedback from trainees. Trainees emerge as highly trained renal physicians, having been supported by a skilled group of established Consultants with a range of subspecialty interests.
The experience gained while attached to the unit is clearly valued by trainees, who highlight in particular the supervision they receive within the department, the supportive environment and the overall level of satisfaction working within a very strong team.
Dr Libby Ferguson and the Palliative care team based in the Marie Curie Hospice in Glasgow continue to provide an extremely high standard of clinical training which trainees recognise with positive responses to the Scottish trainee survey and National training survey.
There is a strong culture of educational governance identified within the centre. Trainees attached to the team there give very positive feedback in all areas, with Foundation trainees in particular highlighting the very supportive and educational environment provided by the team, and General Practice Specialty Trainees similarly appreciating the education and experience that is provided.

Every day our staff and volunteers go above and beyond to provide the best possible care and support to patients, relatives and staff. The Celebrating Success Awards held on 28th May 2025, are an opportunity for us to recognise that, and this year’s winners are fantastic examples of the hard work and incredible dedication all our staff display year round.
Every award winner and nominee should be immensely proud of themselves for the contribution they make to the delivery of healthcare in Scotland.
Find out about the winners and nominees from each award category below.
The winners were also announced live on the night on our social media channels (follow the #ggcawards hashtag).
View our photos from the 2025 Celebrating Success Awards event.

You can read about the previous winners and nominees, watch videos, and view the photos from the awards event using the button below.
If you would like to nominate a person, team or project for an award please complete the relevant form below:
Our dedicated teams and individuals were nominated for the prestigious NHSGGC Excellence Awards by patients, visitors and staff. All of our staff have gone above and beyond in the past year and we asked to hear about your experience of outstanding care and for your nominations.
There are 7 categories in our Excellence Awards and the winners were announced at the Celebrating Success Event on 4th May 2023.
The winners were announced live on the night on our social media channels (follow the #ggcawards tag).
You can find out who the Gold Winners were, read about the Silver Winners who were shortlisted, and also view photos and videos in each of the categories below.
Congratulations to all our winners!
This award recognises staff who provide and contribute towards incredible patient care improving everyday practices across NHSGGC.
Dr Gunn has established the Medical Assessment Unit and Short Stay Unit at Inverclyde Royal Hospital, to facilitate rapid assessment of patients. These are aimed at reducing the number of hospital admissions and ED pressures, while ensuring patients continue to receive the highest standards of care possible.
This has all been facilitated by Dr Gunn while she continues her usual work place requirements, giving up her own time to ensure this was implemented. In addition, she is a focal point for the junior doctors and the advance nurse practitioners and also trainees rotating through the hospital, arranging inductions for these doctors and providing support, advice and supervision as required.


Frailty Advanced Nurse Practitioner Kay Anderson has been nominated for a Better Care award after successfully setting up a primary care focussed frailty service covering every GP surgery in Inverclyde.
By offering polypharmacy reviews and anticipatory care planning, patients are receiving realistic medicine that suits their needs and prevents hospital admissions.
As well as this Kay has managed a Frailty MDT clinic comprising herself, a consultant geriatrician, physio and occupational therapist with links to other AHPs.
Kay’s service has been pivotal in treating patients in the community rather than putting further pressure on unscheduled care services in Inverclyde, with the service dealing effectively with the waiting list for geriatric falls and frailty reviews.

One of Andrew’s patients was going through a high risk pregnancy when her husband sadly passed away after a two week battle with cancer. On hearing the news Andrew called to offer his condolences and also talk about how he and his team could support the patient during this heart breaking time.
Andrew has an incredible way of communicating with patients and their families, with empathy and intuitiveness in abundance.


Over the past two years, the Glasgow Royal Infirmary Nuclear Cardiology Team has launched the UK’s first routine service the assessment of Coronary Flow Reserve (CFR) via Single Photon Emission Computed Topography (SPECT) to reduce Major Adverse Cardiovascular Events (MACE).
SPECT usually involves patients having two 90 minute sessions of intensive imaging, but the team – in collaboration with centres of excellence in Italy and consultants in France – delivered a new technique which can require just one 45 minute treatment, reducing the radiation burden on patients by an average of 30 per cent.
This innovation is a UK-first, with the one day technique being adopted as routine last year.

Due to unprecedented pressures our Urgent and Unscheduled Care services have adapted to new and ever-changing situations which have been nothing short of remarkable. From the launch of the Flow Navigation Centre and Mental Health Assessment Units to the ongoing dedication, commitment and professionalism of our EDs, IAUs, Community Pharmacies, MIUs, in-hours and Out of Hours GP Services, who have worked tirelessly with the support of diagnostic services.
At the start of the pandemic, it became clear that those who became very ill with Covid need a place where they could be seen and assessed safely and away from non-Covid patients.
Our Community Assessment Centres were created. This significant project required input from all of the eHealth teams to ensure the centres had all the necessary telephony and IT kit. They also needed to be set up very quickly.
eHealth teams responded to the needs of the service, working above and beyond to introduce new processes to book in Covid patients outwith hospital settings. The staff showed immense flexibility and changed their hours of work and their roles. The success of the CACs was due to the commitment, flexibility and team working across eHealth to support the Board in its response to the pandemic.
This award commends staff who have implemented an initiative to improve the health and wellbeing of patients, the public and/or staff.
The Emergency Food Discharge Service was created by our Support and Information Services in partnership with the Aroma Café and GGC Foodbanks to help patients tackle the immediate cost of living challenge.
The team uses a referral process from clinicians to ensure no at risk patient or carer goes home hungry by providing a 2-day supply of food upon discharge. The intervention also enables conversations and support in relation to fuel for heating and money to be put in place prior to them going home.
The initiative has supported 1,000 patients as of January this year and is a fantastic example of how our acute, catering and our charitable organisations can work in partnership to meet the most basic, fundamental needs of our patients.


Dr Alison MacBeth, a Speciality Doctor in Breast Surgery at Stobhill ACH Breast Clinic, has almost 10 years’ experience – but she undertook training to enhance her knowledge of menopause in her own time while maintaining her regular clinical commitments.
She is now recognised as a specialist menopause doctor, which has proved to be an invaluable addition to the service, with consultants from other hospitals now referring patients.
Her knowledge is reassuring to patients who attend her clinics, and by liaising with community GPs, she is able to advise on best practice on hormone replacement therapy, particularly in cases involving patients with a family history of breast cancer.


The Health For All Team set a target of improving the health of Unaccompanied Asylum Seeking Young People (UASYP) to ensure they are able to access appropriate health care that meets their needs.
This meant the team carrying out comprehensive health assessments for all UASYP under the age of 18 arriving in Greater Glasgow and Clyde, East Renfrewshire and East Dunbartonshire within 28 days of their referral to the service.
Many UASYP have known adversity or traumatic experiences on their journey to the UK, without any family support. The team sought to address many of the inequalities and challenges the young people faced and have taken on board the many learning opportunities this offered to inform future practice.
This award is for staff who have increased efficiencies taking a new approach to work making better use of resources.
The Cancer Multi-Disciplinary Team eHealth project team based at Glasgow Royal Infirmary have developed a digital solution to help streamline the MDT process, offering an ehealth solution that allows better cross board working and aligns MDT working to standardise referrals.
The project demonstrated its success through a live pilot for gynaecological cancers. In 2022, there were nearly 3000 patient episodes with the feedback from all users resoundingly positive.
This is now being adopted as the standard for cancer MDT’s across the West of Scotland with a matrix of regional eHealth departments supporting the development and support for the application as it is rolled out to each cancer type.

The Knowledge Services Team at Gartnavel Hospital have been nominated for their contribution on the Adult Acute Care and Realistic Medicine apps as.
The team, made up of Michelle Kirkwood, Catriona Denoon, Fran Harkness and Amanda Wright, utilised their skills to organise mass amounts of clinical data into one, readily accessible format for both web and mobile either inside or out of a hospital setting.
Overcoming numerous obstacles, the team have worked to tight timescales and have been committed to delivering an influential and highly usable product.
The Realistic Medicine app was so highly thought of by the Scottish Government Realistic Medicine team, that it has been adopted as the framework and basis for a national Realistic medicine App for all NHS.

Corporate Transport Manager Paul Reid worked through the Covid-19 pandemic to ensure transportation was adapted to accommodate vaccine deliveries in addition to existing regular services.
Since then, Paul has gone on to identify areas where efficiencies can be made with some services, such as the transport of renal dialysis patients, has been brought in-house.
This has meant Paul developing a network of colleagues in various disciplines to develop new ways of working together to improve service provision.
As a result, Paul is now being approached by clinical teams, seeking his advice on how transport services have be adapted to provide more cost effective ways of operating, in-line with the board’s ongoing financial improvement measures
This award recognises the often unseen work of our staff who help make NHSGGC a better workplace, improving the culture and supporting colleagues.

The NHS Practice Education Team have created the Newly Qualified Practitioner (NQP) pathway for all newly qualified nurses, midwives and allied health professionals joining the organisation.
The pathway provides support to NQPs to the organisation throughout their first year in practice by offering a supportive culture and environment as they begin their careers.
By delivering sessions to final year students at university, the pathway informs NQPs of the various support mechanisms in place to allow them to highlight they are joining a supportive organisation which has been shown to lead to improved patient care outcomes and retention of staff.
The team regularly evaluate their input for the supports in place to ensure if any changes are required with the feedback being overwhelmingly positive since the outset.


Rachel is a Witness Support Manager based at West Glasgow Ach and has been influential in providing practical and emotional support and guidance on court and legal process for staff who are required to participate in court or legal proceedings.
Initially, Rachel was volunteering in the role before securing a permanent position to support staff across acute, corporate and partnership settings.
In recent months, the demand on Rachel’s services has increased substantially, yet she has continued to go over and above to provide support to all staff who have contacted her.
Although anonymous, the feedback that has been provided for Rachel has been unequivocally positive as she continues to deliver a unique service.

As part of the Complex Needs Service, Liz went beyond her role as a Health Care Support Worker, and provided extra support to fellow staff members through “Lizzie’s Lunch Club”.
Liz made sure members of the mental health team were able to get a healthy lunch despite their busy daily schedules. She would use her own lunch break to make sure staff were able to eat properly, even making packed lunches for staff on outreach visits as well as care packages for patients, ensuring they had adequate items at their time of need.
Staff said that Liz’s initiative helped them going through their often very busy days and the fact that she is so giving to colleagues and patients was worthy of special recognition.
This award recognises staff who have travelled overseas to provide healthcare and/or education in developing countries or countries in crisis.
Providing healthcare for 1,500 Ukrainian refugees aboard the MV Ambition cruise ship posed a number of challenges – but Senior Pharmacist Katie Earle-Payne’s unique skill set allowed her to help offer outstanding patient care.
Katie speaks, reads and writes Ukrainian and was able to work as a prescribing pharmacist on-board MV Ambition without needing translation services.
She developed pathways for GP support for refugees as well as other specialities and was able to keep refugees accurately informed about treatment as some medicines prescribed in Ukraine are not available in the UK and alternatives had to be identified.
With just two weeks’ notice, Katie worked three days per week on board MV, providing in-person advice and consultations and acting as a link between patients and other services.


The Royal Hospital for Children in Glasgow (RHC) has been twinned with the Children’s Hospital and University of Child Health (CHICH) – a government hospital in Lahore, Pakistan since 2001. CHICH is now the largest children’s unit in Pakistan with 1100 beds and deals daily with thousands of outpatients on very limited resources.
In recent years, the Infant feeding educational delegation has worked hard to help the hospital tackle challenges associated with breastfeeding currently facing mothers and babies. They delivered a 4-day infant feeding programme which was attended by more than 60 staff locally, coupled with a one-day programme of lectures. This is helping create breastfeeding trainers and champions locally and improving outcomes for infants in Lahore.
This type of global collaboration where each member of a partnership benefits is the essence of global citizenship.


MV Ambition cruise ship was berthed in Glasgow, accommodating Ukrainian 1,500 refugees since September last year, until they can find longer term homes across Scotland.
Stewart is the Asylum Bridging Team (ABT) Lead and worked extremely hard, alongside his colleagues, to ensure there was a streamlined system and processes in place supporting Ukrainian refugees to access health care. The ABT were on board the ship providing those residing there initial health assessments, translated information documentation, signposting, and supporting the GP registration process. Stewart was supported by Ukrainian Senior Pharmacist Katie Earle-Payne, who provided medical translations and eased any worries patients had.
As the refugees settle into more permanent accommodation, across NHS Greater Glasgow and Clyde, Stewart and his team continue to support these patients and their GP colleagues.
This award recognises nurse(s) who demonstrate the best qualities of patient care and the ethos of nursing.
Senior staff nurse Charlotte Picken based at the Royal Hospital for Children was the first nurse to identify a need for nurse prescribing in theatre recovery and drive the project through to completion.
After carrying out an audit, Charlotte highlighted the prolonged suffering of children in pain while waiting for additional analgesia to be prescribed by anaesthetic staff. This had a knock on effect by interrupting routine theatre services as anaesthetists were required to attend recovery to prescribe.
As a result, this has reduced suffering of post-operative pain as waiting times for analgesia have significantly improved with additional feedback from nursing and medical colleagues to support this.

Marie has been a Nursing Assistant in Dykebar Hospital for 48 years. She has been based in Continuing care for a great many years, working with elderly male patients with significant cognitive decline.
Marie is approaching 75 years of age and could have retired years ago, but she has chosen to continue working and serving our most vulnerable patient group.
She is committed to maintaining the dignity of her patients, but it is her energy and positivity that singles her out among her colleagues. She brings laughter and joy to her patients and workmates alike.
In addition, Marie knows her experience is invaluable to younger colleagues and she is happy to pass on her knowledge to others. She is very much an “old school nurse” in every sense of those words.


Pamela Charles is a specialist mental health nurse who provides essential support to young people in their homes, completing mental health assessments and ensuring they get the treatment they need.
One day in between visits, Pamela spotted a male on the wrong side of the safety railings on a bridge and immediately she kicked into action.
After alerting emergency services, Pamela used her suicide first-aid training, supporting the individual and eventually talking him back to the safety of the bridge. On that day, Pamela’s quick thinking and compassionate approach helped avoid a fatal accident.
Her response embodies nursing practice. She even continued to her next appointment to ensure the young person she was seeing received the support and care they needed. Pamela herself saw her actions as ‘all in a day’s work’ which further evidences the humility she applies to the way she approaches her job.

The team works hard to ensure every child is re-united with their parents or carers as soon as possible after surgery. Seeing their child go for surgery can often be a hugely anxious and stressful time for families, parents and carers and for a child to wake up and see familiar faces can be distressing.
The staff within recovery understand the difference it makes having parents and carers involved in the process and the benefits of them being re-united with their child as soon as possible. An innovative pager system has been implemented, which allows the team to stay in touch with families and eliminates mobile phone signal issues. This system means the recovery team can meet with parents and carers as their child goes into theatre, introducing themselves and giving any information they might need, putting them at ease.
Recognising people who go the extra mile contributing tirelessly and providing outstanding help and support for the benefit of others.
After seeing a patch of ground at the Larkfield Unit at Inverclyde Royal Hospital, Sandra Forbes set about transforming it into a colourful, tranquil green garden enjoyed by patients, visitors and community groups. With the help of NHS Greater Glasgow and Clyde staff, volunteers and donations from local people and businesses.
While this was the brainchild of Sandra, social worker Fiona McInnes loved the garden and donated some money which helped to transform the courtyard area of the Larkfield Unit, before she passed away suddenly. Fiona is still a key part of the garden and is remembered each day in the garden through a special memorial.

Among all specialties across NHSGGC, our volunteers make among the most significant differences to patients, staff and members of the public.
Margaret Gunduz is a Discharge Lounge Volunteers at the Royal Alexandra Hospital and, without her, patients waiting to leave our care would have a far less positive experience.
The main role of our Discharge Lounge volunteers is to provide companionship and stimulation for patients, offering a distraction whilst they wait to be discharged from their hospital stay.
Margaret is a very welcome extra pair of hands in the lounge, and she has become one of the best-known faces at the RAH. Everybody knows her, and her caring, proactive approach to our patients singles her out as a particularly special member of the RAH team.

The Peer Naloxone Programme was introduced to combat the drug death crisis in Scotland.
It offers training to anyone who might come into contact with someone experiencing an overdose to administer Naloxone which can reverse overdoses and save lives.
Our Naloxone Peer Champions are volunteers living in prisons who are able to provide crucial training on overdose awareness and Naloxone to prisoners and those leaving prison. This service is unique and our champions are helping make the communities that people return to safer and contribute to the reduction of drug deaths in Scotland.
Since November 2021, the champions have trained more than 745 people. There are now 12 champions working in HMP Low Moss, Barlinnie and Greenock and together they are helping equip more people than ever before to save lives.
The local staff awards are popular across all Directorates and HSCPs as they enable all areas to recognise and show appreciation to colleagues who have gone the extra mile. Everyone can give their own examples where amazing care or services have been delivered under hugely challenging conditions and staff have nominated the colleagues who they think most deserve recognition for their stand-out efforts, skills and commitment.
Presentations have been held in each local Directorate and HSCP to award the winners in categories including Employee of the Year, Team of the Year, Leader of the Year, Innovation of the Year and Volunteer of the Year, with the overall winner announced at the Celebrating Success Staff Awards Event on 4th May 2023.
You can find out more about each of the overall winners in each category below, read about the nominees who were shortlisted, and you can also view photos and videos.
Congratulations to all the winners!


The entire multi-disciplinary ED team across both sites works determinedly and consistently to provide quality unscheduled care 24/7, 365 days a year – this is what they do best. The team support each other through staffing shortfalls and significant workload challenges to ensure they continue delivering their core principle of compassionate and safe patient-centred care. A special mention is made to the ED Charge Nurses who work concertedly to maintain an overview of the department and manage nurse staffing.
The full multi-disciplinary team demonstrates a sense of camaraderie, belonging and cohesive working in managing the workload, delivering care, and supporting colleagues in other specialties.


Alison has been a positive and consistent presence in all the wards she has worked in, as well as providing additional admin support to the Rheumatology service over many years.
She is very reliable & organised, supporting colleagues in a cheerful, calm, unassuming and competent manner, and is highly trusted by all those she works with. Her attributes were all the more valued during the pandemic and a time of uncertainty.
Alison knows the patients, familiarises herself with their diagnostic appointments, and is very efficient with all aspects of IT and documentation.
She uses her initiative, communicates updates to families and compassionately cares for distressed patients and relatives.


Donna has shown exceptional commitment to her role both during the pandemic and beyond. Her dedication to her role is admirable, often working in her own time across weekends and out of hours to support patient care, her own team and the wider clinical team in Clyde.
Donna is an example of exceptional leadership within the NHS, always performing her role with warmth, compassion and true professionalism.
Staff, patients and the Clyde senior management team have all benefited from Donna’s leadership which has supported safe patient care, ensuring patients are in the correct clinical areas, and teams supported to make safe decisions in often challenging circumstances.


Dr Wylie and colleague, Dr Torley, piloted, revised and implemented a first Asynchronous Digital Dermatology appointment service (DDAS) in South Glasgow dermatology. This platform became invaluable during the pandemic and has been rolled out to other sectors.
DDAS allows patients to submit images and information of their skin condition, which a consultant reviews and suggests a treatment plan. This has many benefits to patients, including appropriate triage and keeps waiting lists down.
Dr Wylie has also been pivotal in many improvements and innovations with his IT expertise, which is appreciated widely by the Dermatology service and others


Margaret has been volunteering with NHSGGC since January 2020, but has worked in RAH for over 40 years.
In her role as Discharge Lounge volunteer, she provides companionship and stimulation for patients, offering a distraction whilst they wait to be discharged from their hospital stay. Margaret makes every patient feel supported and welcome with a smile and refreshments.
The Discharge Lounge SCN and Volunteer Manager describe their gratitude for Margaret’s generous commitment of time, care and incredible support, which benefits patients, families, department team and volunteer colleagues.
During the pandemic, Margaret was part of the Volunteer COVID Response team, when she contributed several shifts a week, helping with PPE distribution and as part of the valuable Give & Go team.


In leading and supporting the North Sector teams, David has made a significant positive impact on others and our organisational objectives.
He is approachable, supportive and professional in driving forward the goals of the organisation and has co-led one of the board-wide groups helping to shape the Gastroenterology model at GGC.
Always calm and with a smile, David is readily available for advice and guidance and has demonstrated a flexible and listening approach in responding to site pressures and additional capacity requirements.
David’s positive and engaging leadership has helped the site to maintain patient safety at times of significant pressure, in a way that staff feel supported. Thank you David for all that you do for the North Sector.


The ECG Department are completely patient centred in their genuine caring approach, 4listening responding quickly to requests and fitting extra patients on the list. The dedication, hard work, care and compassion of this team have resulted in waiting lists being reduced, appropriate management plans and more timely discharges.
They have created the feeling that teams care about our patients and have demonstrated how departments can work together for the good of our patients and their families. Their teamwork and patient centred ethos is so valuable in to management plans of patients and expediting discharges. If it was not for them the outpatient waiting list would be much longer.
Thank you to the ECG Team, your hard work is an inspiration.

Working together in a true team approach to administer the COVID booster vaccination to in-patients at 3 North Sector sites, this team ensured patients were vaccinated while in hospital in a timely, caring and compassionate manner reducing the risk of COVID infection. They responded quickly to urgent requests, and built up a strong rapport with staff and seamlessly meeting demand despite there own services being remobilised.
Having local staff run the program was beneficial for staff and patients, but it was the patient centred and teamwork nature of this team that made all the difference. Thank you team for your dedication to patient centred care and team working.

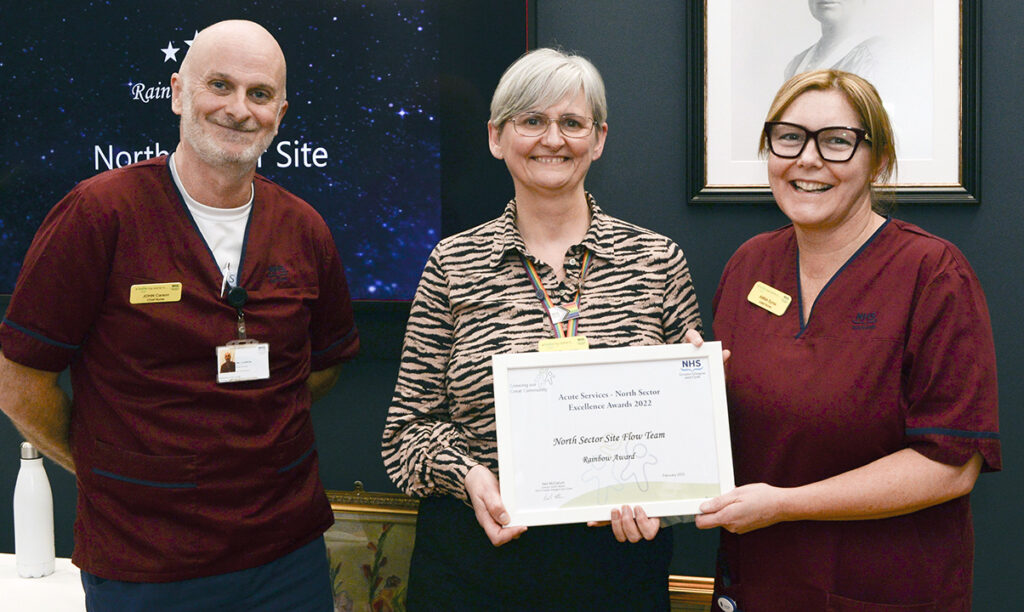
Over the last two years, this team have been an important constant in overseeing safe patient flow throughout the North Sector. Ensuring the management team and on-call managers have all the information required to understand the site UCC and Capacity and Demand position, all in valuable and timely support of patient stepdown and maximising the use/availability of all in-patient beds.
The team work to support wards and are also a key point of contact for staff looking for advice or support. No job is too small and there is a real sense of teamwork, effectiveness and efficiency. Thank you team for being a team that has just made work better for others during such demanding and challenging times.


Thanks to the multidisciplinary team working and flexibility of this team we now have a state of the art robotic system conducting targeted precision surgery geared fully towards high quality patient care and better outcomes.
This technology, and the positive theatre environment created by the team, is giving patients better outcomes, including reduced risk of complications, less time in hospital and shorter recovery times at home. It’s also cutting post-covid waiting times, and impacting turnaround times with less use of High Dependency beds – allowing more patients to be treated quicker.
Thank you team, we commend you for truly living all of our NHS values in implementing the system – in the most challenging of times.


An outdoor rest and relaxation area was created which included seating and tables, where staff can relax and take a break and enjoy the outdoor space. Tricia has done an amazing job in rallying volunteers, resourcing plants and planters. These gardening volunteers have worked hard to turn the garden beds from overgrown weeds to an area full of beautiful and colourful plants/ flowers. Staff regularly comment on the space and the wide range of beautiful plants and flowers on display.
Thank you to all of the staff who gave up their own time to plant, weed and create a beautiful space, demonstrating our values of care and compassion and teamwork, through together creating a space with staff wellbeing in mind.

The FNC team have been in place since December 2020, with the last two year spent developing the service to meet the aims of delivering the ‘Right Care, Right Place, Right Time, First Time’ and provide rapid access to a senior clinical decision maker.
It is an ANP led service led by Mr Ed Pool, supported by Senior Clinical Decision Makers in the form of ED consultant/ specialty doctor. The team use Near Me technology to provide consultations to patients who otherwise would have been directed to EDs across NHS GG&C. The FNC is recognised as a leader for use of Near Me technology with >80% of all consultations carried out in this way leading to improved patient discharge.

With the introduction of total arthroplasty to GGH, Martin has excelled in this role. One of Martin’s main strengths is his attention to detail which means a comprehensive service for his patients – nothing is ever missed and he makes sure he has done everything for patients.
His other main strength is his manner with all patients and the empathy he shows. Following surgery, patients are often sore and the nature of day surgery means that expectation is to get the patient home very quickly. Martin actively listens to any concerns, takes time to explain and ultimately, gets patients on board to get them to achieve their goals and therefore, discharged from the ward.
Martin receives excellent feedback from his patients.

Lynsey is an exceptional Occupational Therapist who is extremely supportive to all colleagues and patients and demonstrated excellent leadership skills in her role. Lynsey became a clinical specialist with Major Trauma in 2020 and since then has been a driving force in developing the Major Trauma and ensuring the rehabilitation journey each patient receives is to the highest standard.
Furthermore, Lynsey is continually taking on students and offering her time to colleagues to help them develop their skills in areas. Lynsey supports colleagues to feel confident in their skills as well proudly advocate for the OT profession and wants the best for all patients which is evident in the positive feedback from patients.

The Emergency Department Research and Innovation team have a number of initiatives that they are leading on locally, regionally and nationally and are becoming one of the leading centres for Emergency department research and innovation in conjunction with UoG Clinical Research facility.
The team’s focus of activity is in devices, data and decisions with work streams in Artificial Intelligence, Toxicology, Radiology, Cardiology and Respiratory.
Furthermore, the team built partnerships with clinicians across specialties to respond to the challenges of unscheduled care admission and rising comorbidity and frailty. The team have showcased their work and presented Scotland, UK and internationally and a number of high impact publications including collaborations across universities, other research groups and multiple industry partners.

Comprising both Imaging and Laboratory eHealth staff, the level of professionalism and commitment of the team has been exemplary, in terms of delivery of key projects and operational support during the pandemic, as well as contribution to the Board’s subsequent remobilisation plan.
Design and implementation of the Regional Whole Genome Sequencing Hub is just one of several examples of their achievements. For patients with certain rare conditions, whole genome sequencing looks at all the patient’s genes in one go. As a result, this test may help to diagnose a condition, suggest treatment options and tell the patient if they have an increased chance of developing a condition and whether the condition could be inherited.
We are immensely proud of our Diagnostics/eHealth Team and congratulate all team members on their brilliant team-working and well-deserved success!

Janice is a Clinical Services Manager in Imaging for the NE and Clyde sectors, with a background in radiography.
She could be described as an exemplary employee who has made a major difference for the delivery of a key objective for the Imaging Service.
During a period of personnel changes that coincided with a Scottish Government assignment that Janice wasn’t previously involved with, and which required a quick turnaround time, Janice became very unwell with COVID, but as no one else was available she ensured this critical assignment was prepared on time.
Janice could have taken to her bed due to her illness but put NHSGGC’s Imaging Service, and the needs of the service, to better serve its patients first.

Laura (Head of Medical Equipment Management MEM) and David (Technical Trainer MEM) are first class examples of leaders developing leaders.
In the absence of Clinical Technologists in the open labour market, “growing our own” talent was the obvious and only choice. They therefore developed an apprenticeship based workforce opportunity to attract, train and retain young people within the MEM workforce to future-proof service delivery.
From it’s inception the programme has evolved from an entry level access programme (entering at B3) focusing only on the engineering apprenticeship framework qualifications at SCQF 6, to an enhanced package of vocational and academic qualifications to meet the requirements for B5 and B6 Clinical Technologists and IPEM registration.
The current MEM programme is the only programme of its kind in Scotland to train clinical technologists.

In collaboration with colleagues in the Gastroenterology Department, the Clyde Biochemistry Team worked to develop and implement the Enhanced Liver Fibrosis (ELF) test assessment pathway. The impact of this small pilot resulted in a reduction the equivalent of 4 Specialist clinics.
Moving forward, early identification allows earlier intervention both to prevent the complications of liver disease and to treat it. It is recognised that half of patients presenting as an emergency with liver disease could have been identified at an earlier stage.
More patients with mild liver disease should also have uncertainty and worry removed until they are assessed, and can be reassured that they do not have advanced liver disease, with advice on management provided in Primary Care.

The aims and objectives of this collaborative working is to ensure that our most vulnerable children and young people receive Christmas presents and food. Christmas can often be the hardest time of year for families who have on-going difficulties including but not exclusively financial hardship, addictions and domestic abuse.
The planning starts early around August time to engage with community groups about giving gifts. Most of the donations are collected by the Community Pay Back teams then sorted into individual gift bags for children of different age groups ready to be delivered to our vulnerable families and groups within our EDC communities.
Around 4000 individual gifts are distributed throughout the Community

Justin is a nurse in the ADRS; in his nomination is a report from a service user’s family:
“The second most valuable resource we found was Justin. He really engaged with our loved one and has guided him through recovery and relapse and continuing on to recovery again. Justin really understands the mental health aspects of the condition and he is sensitive to the needs of family members to be involved in the journey”.
Rab is a Social Work Justice Assistant with the Criminal Justice Social Work Team. He has been described as critical team player, being there for other staff and working well with Clients.
It is evidenced that he has been able to make “Real change with some of the most difficult and volatile clients in the manner that in which he has engaged clients and broken down barriers”.

Lorna has shown her leadership skills in the past 12 months as Senior Addiction worker. Lorna has developed close links with the homeless services providing outreach clinics at First Stop. This has enabled vulnerable homeless people to easily access support with alcohol and drug use. Lorna has provided Naloxone training to ADRS, Justice Services, homeless services and families affected by their loved ones drug use. Lorna has been a key member of the team supporting colleagues and building an effective relationship with both services and services users enabling them to Trust and accept support from services.

This initiative is the East Dunbartonshire component of the overall campaign for the National Naloxone Programme of which the overall aim is to contribute to a reduction in fatal opioid overdoses in Scotland.
Naloxone is a medication that temporarily reverses the effects of opioid overdose, available to anyone at risk of opioid overdose.
The service, through our Senior Community Addiction Worker Lorna Deazeley, has provided potentially lifesaving Naloxone training and resources to 140 people in 2021/22. This has made a significant contribution to the harm reduction agenda, in line with MAT standards. Lorna and the service are passionate about helping the people we support and their families.

This is a group of Care Experienced Young People who are providing support and influencing statutory agencies and corporate parents on working with Young People.
The Champion’s Board was re-launched in March 2022 following a break during COVID-19. Since the relaunch young people have consistently met on a fortnightly basis. The Champion’s Board currently consists of a core group of 14 young people aged between the ages of 15-25, all with care experience.
The work of the “champs” board is making a significant impact across services in East Dunbartonshire by giving them a better insight into the lived experiences of young people with care experience. This enables services to respond appropriately and increase participation and improve outcomes.

Sharon has demonstrated outstanding leadership qualities, she has promoted positive values and shown respect and dignity during a very challenging time while remobilising our Oral Health Improvement Team.
She has shown continual kindness to staff helping to build confidence and resilience, she has developed a culture of dignity and respect which the staff have responded to in a positive way.
Our wider team have taken this culture on board which has resulted in a more positive environment, helped to inspire others to be more patient and empathic towards each other in a particularly challenging situation.
Karen has been recently appointed interim operational support manager to the Oral Health Improvement Team (OHIT). The OHIT deliver national and local oral health improvement programmes.
During this time as interim support manager, Karen has shown great leadership by supporting the department during the re-mobilisation of oral health improvement programmes, and mentoring 3 new team leads by instilling motivation and encouraging all the team to look after their health and wellbeing
Karen’s influence and positive attitude has allowed the team to implement the new Fluoride Varnish dispensing procedures with a reduction in cost to clinical waste and plastics.
Karen is always looking for ways to make working tasks easier and more efficient e.g. promoting sustainability within our Childsmile programmes.

Oral Health Improvement Team and Public Dental Service worked in partnership to deliver the National Dental Inspection Programme (NDIP).
Prior to the clinical team visiting schools to deliver inspections, the Oral Health Improvement Team (OHIT) visited a total of 317 schools to complete a site survey thereby ensuring that the inspection sites were COVID-19 compliant and discuss any changes or equipment required with Head Teachers.
The Oral Health Improvement Team provided assistance not only with completing site surveys but also on occasion prepared the children for the inspection by acclimatisation visits. 317 schools were visited with an approximately total of 14,490 children having been inspected within the time scale of 4 months.

In late, 2021 as the Public Dental Service (PDS) attempted to remobilise dental services throughout NHSGGC, we identified that General Dental Practices (GDPs) had begun to deregister patients, thus increasing clinical demands on the PDS and necessitating a need to increase the number of staff available to work within Emergency Care Dental Clinics.
Therefore, permission was sought to design and develop a Dental Staff Bank to better manage capacity. A Dental Team lead was appointed to support the recruitment of staff and the allocation of sessions to this innovative scheme.
To ensure compliance with GDC regulations Practitioner Registration, PVG and Occupational Health status was checked as appropriate and staff were allocated session within day time and out of hours clinics.

The National Child Inpatient Unit, had never had a physiotherapy resource. A test of change was initiated and physiotherapy commenced with individual patients. Some examples include:

Julie emulates the portrayal of an ideal leader. She is committed passionately to the development of CAMHS services in conjunction with the CAMHS professional leads.
She encourages each individual CAMHS team members, to be the best they can be. Allows individuals / teams to grow, she listens, is solution focused and encourages others to strategically plan and promotes ‘thinking outside the box’. Julie encourages self-wellbeing and a learning culture.
Julie inspires others to work collaboratively and creatively constantly improving and developing the services provided to patients. She promotes a work environment that is respectful, collegial and supportive.
Her Mental Health network spreads far and wide and includes collaborations with the Scottish Government. Julie is an excellent role model and an asset to the NHS.

The GGC Maternity & Neonatal Psychological Interventions (MNPI) service is part of the Scottish Government’s recent commitment to fund perinatal mental health services across Scotland.
The multidisciplinary service addresses the common and/or mild to moderate psychological needs of the maternity and neonatal populations by providing in-patient and out-patient assessments and a range of evidence based psychological interventions.
The central focus in all of these interventions is to enhance the parent-infant relationship, improve parental and infant mental health and to prevent a range of psychological difficulties (emotional and cognitive) in childhood and later life.
The multidisciplinary aspect of MNPI has allowed women to have access to a range of specialist skills so that they receive the best psychological care during their pregnancy and into the postnatal period.


You know you have the winning formula when you are graded as Excellent by the Care Inspectorate.
When East Renfrewshire’s services for children at risk of harm were given a ringing endorsement last year, it was deserved recognition for the joint-working approach across organisations in the area.
East Renfrewshire Children’s Services Planning Partnership is a multi-agency partnership led by HSCP Children and Families along with partners in East Renfrewshire Council.
And this is what the Care Inspectorate said of its work: “We are confident that the lives of children and young people at risk of harm in East Renfrewshire are improving as a result of services delivered by the partnership.”
Well done to everyone involved across the team, for changing lives and being a model for others to follow.


Margaret is an unsung hero who makes a real difference to the colleagues around her. She is a business support assistant in the HSCP who helps with other duties including undertaking minutes for various strategic subgroups. But she does so much more.
When a previous administrator moved to another role, Margaret stepped up to the plate at short notice and took on additional responsibilities within the service.
She did this of her own volition without any training or additional recompense at the same time being under significant personal pressures.
Margaret is always helpful and has a positive attitude and never seeks credit for her work. She is also a carer for a family member and is disabled herself, as well as a dedicated and much-valued colleague.


Clare’s excellent leadership in challenging times has ensured that the staff team at Bonnyton House – East Renfrewshire’s only local authority-run care home – delivers the very best of care and support for its residents.
The emotional toll of Covid-19 on the care sector is well documented, and Bonnyton House was lucky to have someone with Clare’s calmness, courage and professionalism to lead everyone through this period.
She has continued to recruit new staff and support their induction and integration into the team, and a number of the team have progressed into different roles through internal promotion.
In addition, there has been further refurbishment work undertaken to improve the physical premises, all of which has been managed by Clare.
As well as positive comments from the Care Inspectorate, Bonnyton House was awarded improved grades – 2 at Grade 5 (very good) and 3 at Grade 4 (good), testament to the hard work of staff and Clare’s leadership. Well done.


As the COVID pandemic took hold, the need for specialist mental health occupational therapists in care homes became evident to East Renfrewshire’s Older People’s Community Mental Health Service (OPCMHT).
Having identified this gap, Emma Walker, lead occupational therapist and fellow team members, drafted proposals which were approved by senior HSCP management. Funding was agreed for a 12 month test of change post, involving 0.6 whole-time equivalent band 6 occupational therapist.
Positive outcomes as a result of the post included the development of a sensory room to reduce stress and distress among residents. Dementia-friendly ‘pub-like’ signage was adopted to make orientation for residents easier, and dementia-friendly decor was introduced to bring calm to surroundings. For some residents, unsettling moves to other care homes or hospital were prevented after occupational therapy eased high levels of stress.


The team has worked with clinical services across NHSGGC’s hospitals to introduce HEPMA (Hospital Electronic Prescribing and Medicines Administration).
The team built the system, provided training and support to clinical teams, and successfully introduced digitally-enabled clinical change at unprecedented scale and pace.
The HEPMA team has been on hand to provide direct support and training to nurses, doctors and other clinical staff to help them move from paper to electronic prescribing and medicines administration throughout the last few challenging years.
HEPMA improves safety and quality of care by reducing missed doses, eliminating manual transcription of medicines information, and supporting high quality prescribing through electronic decision support. It also enables remote prescribing where clinically appropriate such as COVID wards.


Stewart is a long serving, dedicated and hardworking employee who is always on hand to support with whatever is needed.
He has worked tirelessly over the last few years and has gone above and beyond to enable a smooth transition to hybrid working for eHealth teams. This involved co-ordinating a large number of logistical moves, including specialised equipment in a manner that ensured resilience of systems.
Also to ensure all appropriate security access arrangements were reprogrammed to accommodate the changes and smooth transition for eHealth staff.


Andrew has worked tirelessly over the last few years in multiple areas of eHealth and Diagnostics.
Laboratory medicine is developing very quickly with several high value eHealth projects including Digital Pathology and LIMS procurement. Laboratory diagnostics has also been at the forefront of COVID response and remobilisation which required extensive equipment integration in short turnaround times to support service requirements at scale.
Specifically, Andrew has worked with limited resources on transitioning Digital Pathology from an Innovation Programme to business as usual. This has enabled NHSGGC to be one of the leading centres in the UK for Digital Pathology building the groundworks for Artificial Intelligence deployment.

In conjunction with Pharmacy colleagues, the eHealth Information Management team developed the cohort and mechanisms to identify, contact, and monitor patients eligible for novel COVID treatments in the community to prevent hospital admissions.
Within the space of two weeks the eHealth Information Management team established the eligible cohort of patients utilising data from GP, local clinical submissions, and interrogation of systems.
For launch day, NHSGGC were in a position in advance of other Boards to link local and national test data to establish a bespoke daily proactive text contact mechanism for eligible individuals. Additional developments were established to support eligibility checks and submissions for evaluation.

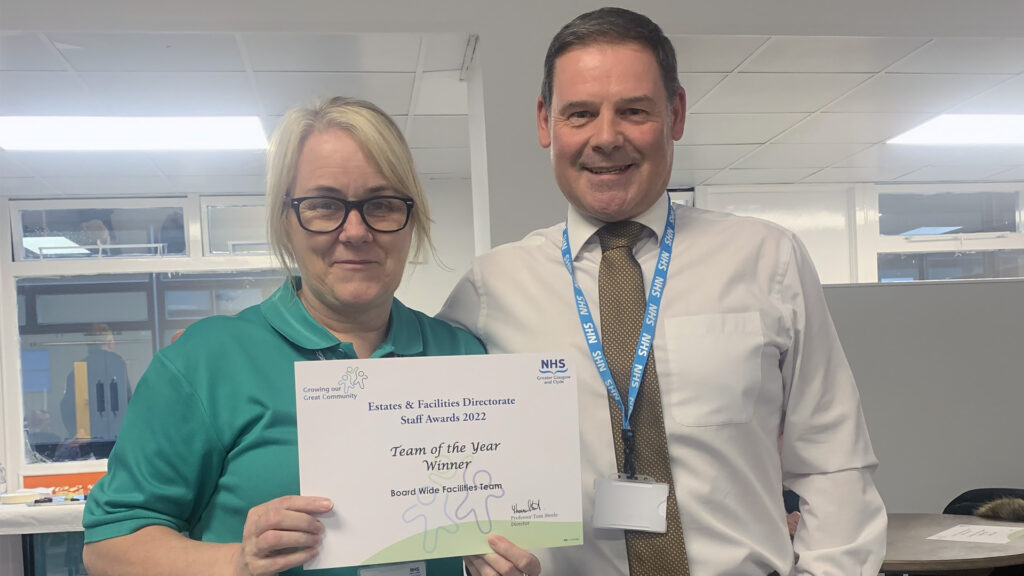
Throughout the challenge of the last 12 months, the facilities teams on all sites have responded to short notice and ever-changing demands to support clinical service delivery. This has required very quick decision making, changes in service delivery models and good communication. This was with a background of a very new senior management team across all sectors where all were establishing new teams.
Worked very closely with clinical colleagues which improved networking, improving communication and breaking down barriers
The sector heads and their teams rose to the challenge, established new networks and ensured the services were delivered.


Thomas completed a number of charity events raising over £8000 for Macmillan Cancer.


This nomination is made to reflect the exceptional commitment and resilience demonstrated by James over a period of almost 4 years, in relation to the upgrade works at Wards 2A/2B in the Royal Hospital for Children at the Queen Elizabeth University Hospital.
Because works were being carried out in a live acute hospital, there was also requirements to minimise disruption to other adjacent wards and services.
James was often required to attend site at short notice whenever any significant issue arose that required mediation between parties, and this was often at weekends and late hours.


As the pandemic started, the Transport Team stood up to deliver a wide variety of services. These included:
The Team were at the heart of the COVID response and recovery. They stepped up when required to allow the patients, staff and the community to receive the appropriate care and attention during what could only be described as unique circumstances.
The Transport Team touched many people’s lives in such a positive manner in a time of crisis.

This is a very small who team who have experienced an increase in the demand for their services at the same time as having to deal with turnover in key roles over the past couple of years. The team supports Board services and the HSCPs and is a key component of the management accounts service within Finance.
They have gone above and beyond to keep work up to date throughout this period through reorganising tasks, improving the efficiency of their processes and doing all that was necessary to keep everything working well and up to date. They have also developed the reporting and increased the knowledge of stakeholders. Contributing to national groups on NHS GGC behalf.

Emma completed her Modern Apprenticeship and has since progressed to new roles within Finance. Firstly in the regional directorate and more recently in North team.
In each of these roles Emma has done an amazing job, picking up new tasks quickly, being proactive and showing great enthusiasm to learn and develop.
Emma is someone who is always looking for ways to help and do more. She has demonstrated a really positive drive to develop herself and add value to the service and the organisation through her hard work and positive attitude.

Gillian is the Head of Finance for the South Sector. She is a shining example to her staff and colleagues through her professionalism, positivity and can do attitude.
Gillian holds the respect of her team, her colleagues and seniors within Finance and beyond.
She has embraced the challenges and opportunities of the past couple of years within the Finance environment and worked hard to support and develop her team. She has put herself forward to mentor junior members of the management accounts team as part of the newly developed finance mentoring programme.
She has supported the mangers within the South Sector with localised budget management training giving encouragement to ask for help. She takes the lead in developing the sectors financial improvement plan suggesting ideas and options for the General Managers and Director to consider.
Gillian takes a lead role in the Sustainability and Value work for procurement and pharmacy working closely with the teams considering options and best value.
Gillian is always willing to lead on new initiatives and work with and support her peers to drive forward changes. She is a dedicated member of the finance team and held in high regard.

Since joining the Board in January 2022, Andrew has overhauled how the Board manages Risk, successfully addressing identified weaknesses in our Risk Management arrangements. In doing so he has also widened knowledge and understanding of risk management across the Board.
He set up a Risk Champions network to support Risk Management work and ensure a consistent approach.
He has significantly improved the reporting formats for Risk Management and his introduction of the ‘Risk on a Page’ format directs focus to key areas and has supported effective risk management discussions taking place.
Fortunately, he has no intention of sitting on his laurels and has plans for further changes and enhancements over the coming years.


The team was assembled in rapid response to the Scottish Government’s commitment to support and resettle Ukrainians fleeing the ongoing war in Ukraine.
The team hit the ground running and have been responding and adapting daily to the everchanging situation where children and families are arriving in Glasgow with minimal possessions, often exhausted after long journeys.
The team have been successfully matching individuals to sponsors in the community who have stepped up to support Ukrainians in their own homes. As a very new team responding to a unique set of circumstances, staff have adapted and responded to emergency situations on a daily basis, providing an empathetic and sensitive response to people who have experienced extreme loss and trauma.
The team have been on hand daily as a point of contact to provide consistency and advice to help people adapt and integrate into life in Scotland.


Ian is a longstanding member of the Mental Health Team at Florence Street Mental Health Resource Centre, providing social work services to the south of Glasgow.
It’s said he has a fountain of knowledge and is always willing to share this with others.
Ian, who has strongly retained his social work values, always makes himself available to service users in crisis, responding in a way that is supportive, considered and without judgement. He has an in-depth understanding of mental health and wellbeing.
Ian has not let increasing demands impact on the service he has provided and has even written poems and helped secure a university placement for a service user who has no family and has been impacted by deterioration in their mental health.


Anna’s support and enthusiasm has been inspiring to her team all through the pandemic, whilst ensuring vital services for service users continue. Her team say she has outstanding leadership qualities and is always able to offer appropriate and clear direction when its needed.
She organised an induction programme for colleagues who joined the team during the pandemic recognising how difficult it was for these new team members to integrate at a time where they were unable to physically shadow others; to build their networking; and to meet their peers.
Anna’s role as team leader has been a critical part of the business for strategic planning to promote transformation in shifting the focus to ensure partnership working and enabling and supporting older people to remain at home.


The COVID-19 pandemic had a significant impact on how our five residential care homes for older people delivered services.
A key priority for this critical care service has been our staff mental health and well-being and helping them remain both physically and psychologically well to cope with the extraordinary demands and pressures within a very stressful and often emotionally charged environment.
In collaboration with psychological services of NHS Greater Glasgow and Clyde, they developed a “20 Minute Care Space” which all 755 staff were able to access day and night – to reflect on lived experiences with colleagues. It’s since been recognised as an area of Excellence in Best practice by the Scottish Government and Care Inspectorate and rolled out across other Care Homes.


The Peer Naloxone Programme provides an opportunity for those who live in prison to participate in a coordinated and supported approach to a peer supply model of Naloxone. Peer mentors were recruited to support the peer delivery of Naloxone Training and distribution.
This service is unique, and the mentors have contributed to saving lives and reducing drug deaths recorded in Scotland.
Peer Champions participate in a number of training sessions. These training sessions equip the mentors with the knowledge and skills to carry forward their peer mentor role.
Peer Champions provide evidence-based overdose prevention messages, help to dispel myths and encourage safer drug using practices. Peer Champions offer Naloxone training and issue Nyxoid (Nasal Spray Naloxone) to their peers the night before liberation.

The NHSGGC Recruitment Team have put into action a new approach to increasing candidate engagement for registered and non-registered Nursing/Midwifery staff.
This work was necessary to find a solution to expand the current recruitment pathways to address the recruitment challenges that have surfaced particularly over the pandemic period and post pandemic. Most specifically those challenges in either ’hard to fill’ nursing /Midwifery specialties or geographic locations.
We have had the opportunity to share our skills with other NHS Boards either through helping them use our expertise in the Job train recruitment system reporting functionality, and the great success achieved through supporting the Scottish Ambulance Service, realigning their Mobile Testing Unit Staff to HCSW Roles with GGC.


Nicola has demonstrated outstanding support to the Test and Protect Transition Workforce Group enabling NHSGGC to effectively manage a range of complex workforce issues involved in the cessation of a significant temporary service under a high level of public and political scrutiny.
The scale of the task, along with the range and complexity of employee relations issues involved, was at times challenging. She showed great resilience, dealing confidently and competently with all stakeholders, building strong relationships with staff partners and supporting local managers, as well as dealing sensitively with staff facing the prospect of their GGC employment coming to an end.
Nicola has shown excellence in HR practice which is worthy of recognition.


Lisa takes complete ownership of the medical bank. She knows virtually every doctor on the bank individually, and equally knows every service manager and roster co-ordinator.
Lisa makes it her responsibility to recruit additional medical staff regularly, in particular enrolling new junior doctors when they rotate into GGC, encouraging them to join directly with us, rather than work via an agency.
She is hugely passionate about her job, quietly driven to fill shifts, with an unparalleled set of moral and ethical standards.
Lisa’s approach to her work, the manner in which she conducts herself and perhaps most importantly the quiet way in which she leads, encourages, coaches, motivates and supports her team is remarkable.


Mathew, Heather and Fergus approached international recruitment by providing a bespoke service attracting candidates from identified talent pools, providing person centred support and guidance to successful candidates through interview, and on boarding and induction.
The team successfully advertised, registered interest, arranged and supported interviews, and on boarded 50 internationally trained nurses.
The team provided an immense amount of support to the nurses, helping to arrange air travel, airport transfers, accommodation, training, etc. The team also provided support to the services who received the new recruits.
NHSGGC were the only Board to successfully recruit internationally trained nurses.


During Winter Wellness Week staff/teams were encouraged to take part in various health and wellbeing competitions.
The team and those they support, virtually travelled to Japan to accomplish the Mount Fuji challenge. This took the staff and service users on a 46-mile (74km) journey around the Fuji Five Lakes and up to the peak. Their steps and distance were calculated including swimming, walking and carrying out physiotherapy exercises.
Over the week the team completed the challenge twice, on the third attempt they made it up, but didn’t manage to come back down, but felt that this was okay as the views are magnificent!
Everyone enjoyed it so much that they have decided to keep going over the coming months!

Fiona has demonstrated exceptional commitment to the children and young people of Inverclyde through her hard work in speaking to children and young people where welfare and/or child protection concerns have been raised and completing assessments that keep their voices at the centre.
She has supported many families through extremely difficult and complex circumstances, always demonstrating empathy and patience.
Fiona’s standard of report writing, assessment and analytical skills are consistently of an excellent standard.
Fiona’s contribution in her role has been outstanding and is difficult to summarise the positive impact she has in the Service.
She is a highly valued member of the team who has always contributed positively and with empathy and careful consideration as to the best interests of the child.


Loranda has worked within the Inverclyde Community and Specialist Community Paediatric Team for 20 years she has shown her ability to be a flexible, dependable, innovative leader who grows and develops to meet the changing needs of the population of Inverclyde and the service.
She has worked and excelled in compassionate leadership as role model and influencer on community children nursing, supporting children in their homes with complex needs, including palliative care at home, to integrated working with acute sector, with ambulatory care and outpatient provision at L North, Inverclyde Royal Hospital, to disability nursing services for new and review referrals for children with complex needs in school and community clinics, to laterally neuro diversity and childhood autism assessments.


Despite the restrictions and adversities of the pandemic, the occupational therapy service has demonstrated resilience, ingenuity and determination to successfully achieve a new face-to-face group for people living with dementia.
Journeying through Dementia is an occupation-based group programme that aims to support people at an early stage of their dementia journey, to engage in meaningful activities and maintain community connectedness.
Throughout all the co-creation activities, people with dementia were clear that they wanted to have the opportunity to access groups that offered practical advice and support of how to continue to live well with the condition. The aim of the program is to promote continued engagement in meaningful activity by equipping individuals with the knowledge, skills and understanding of ways to do the things they enjoy for as long as possible.


This group of volunteers selflessly gave their time in very difficult circumstances during COVID lockdown when many stayed at home.
Throughout, the volunteers worked closely with HSCP Learning Disability service to deliver hot meals to isolated and vulnerable people in the community, this complimented HSCP staff and other groups of drivers.
They continued to transport service users, HSCP, and third sector staff to locations where they would be supported during the day, while adhering to infection control measures.
From March 2020 the volunteers and escorts have been integral to the delivery of the HOME1st Transport pilot and have transported patient’s home from hospital, to and from care home respite, and other locations.
They have never refused a Transport request from the HSCP Dispatcher and have worked hard throughout, often at short notice and weekends, without hesitation.


All three team members provide a mixture of in-patient and out-patient support at clinics to relieve consultants and waiting list pressures for rheumatology patients.
They have changed patient pathways to make drug delivery easier, give regular advice to the nurse specialist team for help line enquiries and home care issues, and responding to anxieties over COVID, vaccines and the many other issues that accompany immunosuppression and biologic drug therapy.
They perform clinical assessments of joints and skin and prescribe biologics and adjuvant therapies. One team member is now also doing joint injections to ensure a “one stop” clinic. In addition the team have made significant financial savings in medicines through biosimilar switching and tapering of biologics.


Amanda is dedicated to her profession as a pharmacy technician. Her constant drive to improve the department is inspiring.
She has lead on projects including near miss recording and education and training of new staff.
Amanda is the main link between pharmacy and specialist consultants and has ensured continuity of supply of medicines throughout the pandemic.
She is a fantastic example of a patient centred pharmacy technician with a passion for quality improvement.

Nathan provided pharmacy input to the Monkeypox outbreak and vaccination programme.
He implemented medicines governance processes within Sandyford.
Nathan explores ways for Pharmacy Public Health to develop into other priority areas.
He is an elected president of GHP, a true team player, and an emerging leader.
And always with a smile!


Jenny is a brilliant leader who truly cares about her team. She has pushed us all to develop further and made sure we have learning opportunities available. She undertakes a massive amount of work for one person. She is kind and considerate and makes us all feel supported at work.
She has been involved in developing new heart failure clinics and encouraging all of us to upskill ourselves to be involved in these so we are more visible to the patients. This has also helped us get more variety to our working week.
Jenny always leads by example. She supports all individuals in their development, encourages us to participate in decision making and is currently progressing the team’s clinical roles.


In February 2021, as part of the GGC Surgical Remobilisation Programme, funding was secured to trial a pathway of pharmaceutical care and medicine supply at selected sites.
This was undertaken by two experienced pharmacists and included development of an arthroplasty service at Stobhill and pre-operative review clinics for all sectors in GGC.
It utilises new ways of working, digital solutions, demonstrates advanced practice and has the patient at the centre of the process. The project has demonstrated improvement in patient care with significant reduction in post surgery healthcare encounters. This service is proactive rather than reactive, demonstrating cross boundary working and has improved job satisfaction for those undertaking this role.

For delivering excellent patient care and leading the way nationally. This service is a government driven priority for NHSGGC and provides treatment for the patients at highest risk from COVID-19. Service pressures in all areas of healthcare and the complexity of the medication due to drug interactions meant other professions felt unable to take on this role safely.
The whole pharmacy team across acute care, primary care, community pharmacy, clinical trials, governance, PDC and specialist services came together to deliver a 7 day a week service assessing and treating patients with medicines delivered to their door under tight time pressures.
Patient feedback has been excellent.


The T2D Hub supported the design and implementation of a pathway for newly diagnosed T2D patients into structured education, weight management, live active and smoking cessation support.
The hub contact all newly diagnosed patients and through motivational interviewing techniques, encourage them to engage with services. They have delivered an excellent quality of service to a large volume of patients. Since the launch of the pathway there have been approximately 90 new diagnoses each week. Alongside these patient contacts, the Hub staff work across a range of eHealth systems enhancing the Board’s use of Sci Diabetes, coordinate the T2D education programme timetable and respond to a range of queries from clinicians.
Award collected by Rose Scullion, T2D Pathways Facilitator and Marjorie Innes, Structured Education Training Coordinator on behalf of the T2D Hub.


Kirsty has consistently gone above and beyond to ensure the staffing and smooth running of the busy vaccination clinics. She has been praised for her flexibility and hard work as well as her ability to cope with conflicting demands on her time.
Kirsty has been instrumental in ensuring the safe delivery of clinics, managing the many pressures placed upon the service – avoiding the potential cancellations of many appointments.
Kirsty demonstrates patient centred care, not only for any patient coming into a clinic but also for any staff member involved in the community vaccination programme.
In an ever changing landscape and with new guidance/challenges experienced frequently Kirsty has always been positive, inspiring and an excellent team player
Award presented to Kirsty Howie, Team Lead for Adult Immunisation.


Claire Marie was key to the planning, preparation and delivery of the Naloxone Peer Mentor Programme in HMP Barlinnie and HMP Low Moss. The programme was developed to support the reduction in deaths in Scotland attributable to drug use and consists of people living in prison offering Naloxone training prior to a planned liberation date and issuing the individual with a supply of Naloxone Nasal Spray (Nyxoid).
Clair Marie demonstrated her compassion, empathy and enhanced emotional literacy through her communication with multiple stakeholders and engagement with the peer champions.
Peer Champions report that Claire Marie’s support made participating in the programme much easier and felt respected and valued as a mentor, a volunteer and a person.
Award presented to Clair Marie Blair, Health Improvement Practitioner


Naloxone Peer Champions were recruited by the Health Improvement Team in Prison with the support of the Scottish Prison Service.
The aim of the programme is to support the peer to peer delivery of Naloxone training and distribution to people about to leave prison. Developing and supporting peer to peer Naloxone supply is not new to NHSGGC, however it is an entirely new approach for people currently living in prison.
Peer Champions meet with everybody returning to community and not just those who are engaged with addiction services in prison. This increases the availability of Naloxone in wider communities.
People left prison more equipped to support others in their families and communities to be safer whilst engaging in drug use.


Naloxone Peer Champions were recruited to support the peer delivery of Naloxone training and distribution to people leaving prison. This service is unique and our mentors have had the opportunity to influence the number of deaths recorded in Scotland which are attributed to substance misuse.
We currently have 14 volunteers across Prison Health Care (PHC ) in HMP Low Moss and HMP Barlinnie. Since the project went live, we have delivered training in overdose awareness and the use of naloxone to 473 people leaving prison and returning to communities across Scotland. 83% of these people accepted Naloxone for the first time.
Award collected by Katie Yuile, Health improvement Assistant Practitioner on behalf of the Peer Champions

Led by Senior Charge Nurses Kirsty Etherson and Theresa Shaw, these two medium secure female ward teams work tirelessly and compassionately to provide a safe, secure, person-centred and therapeutic environment and interventions for female forensic mental health patients.
Excellent high quality, non-judgemental care delivered jointly is the norm as a result of the desire to rehabilitate, care, think creativity, and risk manage on a consistent basis.
For our patients this means that they feel safe and secure and cared for, for some patients this is the first time they have received such care, compassion and emotional safety in their lives and for carers they feel reassured and supported that their loved one is receiving high quality care.

Oudwin is responsible for the Nursing Team in the Interventional Neuroradiology Service, and over the past year has taken on a number of additional responsibilities, including playing an instrumental role in integrating a seamless in-patient Mechanical Thrombectomy pathway, and coordinating training days for all staff.
This has resulted in increased awareness/engagement across multiple specialties and confidence within the INR team, providing great benefit to patients.
Every day, Oudwin goes above and beyond for our INR patients.
Having worked in a number of departments across the country, our patients are very fortunate to have an exemplary pathway, from the time they are seen in clinic, pre-assessment, procedure day, and post-operative care extending to meticulous checks when our patients are discharged home.

Lynsey and Leann are two examples of highly motivated and compassionate nurse leaders who strive to deliver the highest standards of person centre care for patients within their respective services.
Leann is known throughout Rowanbank for her outstanding commitment to her patients, her team, and wider services every day, but, most of all, throughout the pandemic. Colleagues who worked with Leann during COVID-19 speak about the absolute joy and delight of working with her due to her tenacity and strength of character.
During the pandemic, Lynsey and her team went above and beyond to ensure that care was exemplary, person centred, safe and effective during the unprecedented situation that they and their patients and families faced. As a result, many patients and family members have positively acknowledged the highly valued care and attention that they received on the Care Opinion web platform.

Audrey works in a research role as part of the Beatson Practice Development, Education & Research Team.
Following an external assessment process to retain a national quality standard, she received a small grant from MacMillan Cancer Support for a Creative Arts Project in the Macmillan Day Bed Unit, with the aim of producing a relaxing and comfortable environment for patients, whilst engaging patients and staff in the development and use of art.
The project resulted in a variety of wonderful art work being received from both patients and staff including drawings, paintings, poetry and collages, together with some lovely stories and inspirational messages which were displayed in the main waiting area.
A brochure was also prepared for World Art Day and the project featured in the What Matters to You day.


Mirin and Milldale Day Opportunities, are two of our Adult Learning Disability Day Services. The teams support adults with learning disabilities to live their lives as fully as possible. Normally this is facilitated using their building bases and integrating with other community groups.
The Teams continued to deliver services to Renfrewshire’s most vulnerable residents throughout the pandemic all while creating and adapting to new ways of delivering the service including technology.
They enabled service users to enjoy something akin to their normal service while allowing their parents/carers to maintain some of their routines. Staff were constantly providing reassurance, counselling and promoting a positive atmosphere to allow the lifeline service to continue.


Douglas has worked for Renfrewshire HSCP since 2009 as the Choose Life Suicide Prevention Coordinator. His personal attributes include hard working, proficient, and dynamic innovative and demonstrates this within his day to day work.
Douglas makes a significant difference to not only the staff, but the people of Renfrewshire.
As an organisation, we are lucky to have Douglas lead on Suicide Prevention for us.
Douglas recognises that suicide prevention is a community issue, therefore when addressing this he reaches beyond mental health services. This is achieved by offering suicide prevention training programme to “anyone who lives and/or works within Renfrewshire”, as well as engaging community groups and other wider initiatives.


Patricia is a remarkable individual. During the pandemic, she put in long hours supporting staff, families, and residents by listening to their concerns, emotions at a time that was very distressing.
She is a dedicated manager who gives every task 100% and more. Patricia ensures staff have the opportunity to re-evaluate practice skills so that going forward they excel in their job.
Patricia broke her foot last year, but still came to work so that she could support the staff in any way that she could.
Admiration is a word many would use, she is a hard worker, reliable, honest and nothing slows her down.


The Community Safety Team support wider agencies within Renfrewshire, providing easier access to mental health services.
As a team of Mental Health Nurses, they have made such a difference for other services having access to a mental health resource, providing support to wider staff network within Renfrewshire. They also hold a caseload for individuals to complete short term pieces of work and support individuals in mental health recovery.
Together they demonstrate great teamwork, effective communication, expertise and decision making whilst providing high quality recovery focused patient care and interagency working.


Gateway is a registered service which offers a therapeutic environment for individuals with Autism, complex needs and learning disability.
Gateway introduced an initiative called ‘It’s a Game Changer’. They looked to find innovative and creative ways to link up with council lead initiatives and local organisations to explore greater community involvement. They aim to remove barriers and overcome obstacles and difficulties with inclusion.
Gateway boasts a dynamic staff team that goes above and beyond what is expected of them, to meet high outcomes and goals for the people they support. They are highly skilled, trained, motivated, creative and innovative team.


Angela is an asset to the HSCP. She shows drive and commitment every day in the delivery of Renfrewshire’s Primary Care Improvement Plan and our clinical care governance arrangements.
She consistently goes above and beyond to provide the best possible support to colleagues and GPs, with a consistent focus on improving outcomes for local people.
All of Angela’s colleagues continue to praise her contribution and recognise that they could not do their own jobs without her input.
We cannot praise Angela’s approach highly enough through her commitment to getting the job done, often working long hours to do so, and her ability to find innovative and pragmatic solutions to really challenging issues for our frontline and community-based services.


Everyone speaks highly of James, and are in awe of his knowledge and expertise, and his ability to know the right person to contact for any issue big or small.
It’s hard to explain the difference James makes, as it isn’t just one thing, it’s a combination of all that he does and how he does it.
Over the past couple of years he has been instrumental in ensuring PPE was available for both our own staff and our external providers – including phone calls late at night and at the weekend to source supplies when they were at risk. He has also stepped in to cover a number of roles over the period as well as still managing to do his day job.


This Team has shown remarkable adaptability and resilience during a very challenging 2 years.
Early in the pandemic, they volunteered to work in front line roles in the COVID Assessment Centres, and Track & Trace.
However, Diabetic Eye Screening is a national service and, when it recommenced in June 2020, there was a considerable backlog of patient appointments.
The Team’s response was to go above and beyond what was expected of them, introducing innovative solutions which resulted in almost double the number of appointments available to patients each month.
This amazing effort involved the whole team – both administrative and clinical staff – who showed passion and pride in their Service, and proved that working together really does make a difference.


Liz Kerr was an integral member of the project team during the planning, construction, commissioning and move to the new Clydebank Health & Care Centre – even collaborating with the build team to choose the colour schemes, flooring and furniture to create a pleasant work environment.
Liz’s commitment, decision-making and hard work all contributed to the build completion. During the commissioning of the building, she led by example, often taking a very hands-on approach to ensure that everything was where it needed to be. Given that much of this took place during the pandemic, the challenges were huge.
And all of this was achieved whilst still doing her “day job” of managing and supporting the very busy HSCP Community Admin Team.


As the Manager of Blairvadach Children’s House, Alexis has demonstrated great strength and resilience during the challenges of recent years.
She leads by example and has the ability to inspire and motive her Team to reach their full potential. The result is an environment where the young people have the opportunity to thrive – an achievement acknowledged by the Care Inspectorate who gave Blairvadach the highest award, citing it as an ”exceptional model of practice”.
Alexis is regarded by her colleagues as a caring, respectful and approachable manager whose motivation has always been the high quality care for the young people.
Her success is based on a philosophy of “giving” and she consistently invests her time and skills in supporting others.


Elaine Allan, a Senior Paediatric Occupational Therapist, was concerned at the impact of “Lockdown” on children. She recognised that young and vulnerable children with significant additional support needs had not been able to prepare for the transition from Early Years to Primary School.
Working with Kilpatrick Primary School and Early Years’ Service, she secured funding and collaborated with parents, Nursery and Primary 1 staff, to develop resources to support the children. In addition, she created a “passport” style document to share the information with their new schools.
Positive feedback from all those involved demonstrated the value of this initiative to the children, their families, and Education professionals – and the tools and resources can be used again, year after year.


This team, when faced with an atypical and challenging delayed discharge demonstrated even more care and compassion than usual and collaborated with other teams and colleagues to provide care above and beyond their abilities by adapting to the situation and learning new skills. They provided impeccable care for a CAMHS patient, with significant additional needs, aggressive behaviour and no family engagement, who due to social circumstances could no longer be cared for at home.
Thanks to their flexibility, resilience and teamwork, the patient remained in a safe environment, with all needs being met, while trying to find an appropriate placement, as well as advocating for the patient.
Thank you for going above and beyond to ensure high quality patient care.

Stevie is a Health Care Support Worker in Children’s Theatres, who is considered the backbone to the team for their positive work ethic and expertise, forward thinking and planning, supportive teamwork values, extensive equipment knowledge, good sense of humour and reliability.
Stevie’s equipment knowledge is so good it often surpasses the knowledge of consultants and really supports the newly qualified nurses with as well. Stevie’s work ethic, values and knowledge create a positive environment and good “karma” in Theatre, which contributes to the whole team functioning better and everything flowing well, which is of huge benefit to the team and to our patients.
Thank you Stevie, for everything you do for the team and our patients.


In the roles of Gender Based Violence (GBV) and Social Work Liaison midwife, Anne has worked to reduce the impact of vulnerability on the unborn child.
Ann has an amazing manner when liaising with police, collaborating with multidisciplinary health professionals, the special needs in pregnancy team, patients themselves and updating on child protection issues. Her efforts and focus on early intervention result in higher quality care plans that meet vulnerability needs, robust documentation and awareness that result in improved outcomes for mums and babies.
Thank you Anne for safeguarding our patients, cultivating and maintaining great relationships with child protection and social work stakeholders, upholding information sharing and data protection, and for being a pillar and role model for the team.


Christine is an experienced Senior Charge Nurse and a fantastic role model in leading Gynaecology Ward 49 at QEUH, especially through some challenging periods.
As well as ensuring that all elective and emergency Gynaecology patients receive high quality care, Christine has worked closely with DME colleagues to ensure that DME patients receive a high standard of care.
In addition to ensuring that all patients, carers and relatives are treated with care and compassion, Christine has also maintained a focus on the wellbeing of staff and ensuring that everyone is fully supported.
Thank you Christine for enhancing patient experience on a day to day basis, and for engraining care and compassion for our patients, and each other, within Ward 49’s culture.


This team have successfully delivered a new i131 MIBG ionising radiation service in Scotland, where patients can receive treatment closer to home and no longer have to travel to England for treatment.
This involved a multidisciplinary team working effort, sharing expertise and knowledge to ensure that all safety needs were met to deliver this care to patients within Schiehallion Ward 2A at the Royal Hospital for Children in Glasgow. This included developing Standard Operating Procedures, Health and Radiation Safety, Debrief processes and a massive training programme run by the Ward 2A Educator.
Thank you to the team for working together to develop this new service in Scotland, with the best patient experience and patient and staff safety top of mind.

The support provided by the GCHC Volunteers is both seen and unseen, and provides such a vast coverage of assistance many will never be aware of the help gifted.
Our team of Volunteers step up to help our patients, their families and our team whenever called upon. With tasks such as, collecting and delivering, keeping our patient gardens and parent facilities in tip-top condition, supply of essential refreshments, play support to our patients both in hospital and at awareness events and in supporting fundraising that allows the Charity to gift so many benefits to the hospital.
We thank each and every one of our Volunteers from the bottom of our heart, you represent the heart and soul of our hospital.


June is a Lead Clinical Pharmacist and her work on the management of clinical guidelines has been outstanding.
Obstetrics, by nature has a vast amount of guidelines, that need to be available for staff at any time and the archiving process of guidelines is particularly important as when looking back at care, staff need to be able to access the appropriate guideline of the time.
June has been instrumental in the process of organising, archiving and maintaining accurate guidelines. Thank you June for going above and beyond your role to clear the backlog of paper guidelines that needed archived, ensuring that our staff have easy access to new guidelines and ensuring that old ones are taken down and filed appropriately.
The team, department, service or function that has been judged to have worked together as a team and made the most significant contribution to quality of care, population health and care, service delivery or staff wellbeing likely under significant pressure or difficult circumstances.
Any member of staff who has stood out as an exemplar of care giving, service delivery or who has made a major difference for colleagues around them or the delivery of a key objective for their department or wider NHSGGC/HSCP.
Any member of staff who has demonstrated outstanding leadership, positive values and behaviours and/or inspired others in a particularly challenging situation, or for the respect they get from others through the day to day difference they make for those around them as a leader.
Any member of staff can demonstrate leadership, not just those who formally manage people.
To recognise any individual, team or department responsible for developing and implementing an innovative service, method, technology or process that has made a significant difference to quality of care, wider population health or care, service delivery or to the wellbeing of our own staff or to the efficient use our resources.
To recognise an individual or team of individuals who have volunteered significant time and effort to the benefit of our patients, service users or staff and made selfless contribution perhaps under difficult personal circumstances.
Medical Director, Dr Scott Davidson, in collaboration with The Royal College of Physicians of Edinburgh, will once again present two prestigious awards for Medical staff.
The William Cullen Prize for excellence in teaching and a separate William Cullen prize for service innovation will recognise a clinician, or clinician and team, as having made a significant contribution to local teaching or service innovation in Greater Glasgow and Clyde.
The winners of each Prize will receive a framed print of a William Cullen letter which will be selected from the Royal College’s archive. The William Cullen Prizes will be presented at our Celebrating Success Event.
William Cullen (1710-1790) began his career as a medical lecturer and pioneer teacher of Chemistry at Glasgow University rising to international fame as the leading figure in Edinburgh University medical school and served as president of the Royal College of Physicians of Edinburgh. He was appointed the King’s Physician in Scotland and became the most influential medical lecturer of his generation. His private consultations survive as a remarkable archive of several thousand letters.
We currently have recognition awards for medical teaching based on performance in the national trainee and student surveys. The overall William Cullen Prize winner will be selected from that cohort of around 20 of our top performers.
To enter or nominate for the William Cullen Prize Innovation award please complete this form. Dr Davidson and a panel of senior medical staff will form the judging panel.
Closing date for nominations was Wednesday 16th April 2025.
The annual Local Staff Awards enable Directorates and HSCPs to recognise and show appreciation to colleagues who have gone the extra mile. This has been particularly relevant in dealing with the pandemic which has tested the resolve of all our staff in their ability and capacity to cope under extraordinary circumstances.
There are five main categories within these awards, however, there may be alternative or additional awards within the directorates or HSCPs.
Congratulations to all the winners and nominees!
The awards were presented at the virtual Celebrating Success Awards held on 23rd February 2022 which you can watch on this page further below.
You can find out more about each of the overall winners via the video links below, and read about the nominees who were shortlisted.
The awards were presented at the virtual Celebrating Success Awards held on 23rd February 2022, hosted by Professor Jason Leitch CBE, National Clinical Director.
Everyone can give their own examples where amazing care or services were delivered under hugely challenging conditions. Staff nominated the colleagues they felt most deserved recognition for their stand-out efforts, skills and commitment.
Read more about each of the nominees below:
The Estates Team are regarded as the ‘unsung heroes’ of IRH site. They demonstrate true commitment, pro-active efficiency, planning and fast responses to requests from across the hospital.
During the pandemic, the team were key to enabling structural changes needed to ensure safe clinic areas and patient pathways, including for example, expansion to ITU within the theatre area, front desk area within the main entrance, extensive floor markings and signage. The Team also oversaw the co-ordinating & enabling of a major power supply project, working closely with clinical colleagues to ensure minimal impact to clinical care & continued smooth running of the site.

Sandra is described as a passionate & committed OT who regularly goes above & beyond to meet patients’ needs.
In a bid to create something positive during the bleak time through Covid, Sandra decided to transform the courtyard garden area between Ward 1 & Day Hospital in the Larkfield Unit, and established the Rainbow Garden.
She recognised the therapeutic benefits of the garden and that it would provide a tranquil and secluded environment for patients, visitors and staff. It has been used regularly since the improvements were made.

Claire is truly supportive personally and professionally to her team members, who work in a particularly stressful board-wide specialty.
This has been especially evident during Covid, when Claire has made a significant contribution to patient care and the wellbeing of colleagues.
She is regarded as having a can-do and solution-focused approach to her role and in the way she manages the Palliative Care service.
The nomination for Claire included a personal account of the support she provided to a new colleague and their appreciation of the ways in which she helped them integrate into the team and address workload challenges.

The team developed a new protocol to support critically ill patients with SARS-Cov-2 who required RRT (Renal Replacement Therapy).
This was an alternative to the approach implemented by other units, and involved increased citrate for patients, and sought to balance the benefits of preserving filter cartridge lifespan and risks of anticoagulation associated bleeding.
Intensive support was provided by John as Practice Educator, who personally supervised operational issues, at a time when clinical activity was immense within the unit. The study showed an increase in filter life for patients on an increased citrate dose, without any adverse outcomes.

The Volunteer teams provide valuable support to staff, patients and families in the Clyde hospitals, including in wards, Give and Go service, and staffing the Royal Alexandra Hospital Staff Rest and Recuperation Hub.
The Sector felt it was important to specifically acknowledge Harry Balch, who expertly guides the teams, responding quickly to the requests from services, ensuring well organised and co-ordinated support is directed where it is needed most.
This was especially true during the pandemic, when many new volunteers came on board, and Harry had to ensure they worked within safe protocols, felt confident in their roles and were effectively supported.
Dr Aleks Marek is playing a pivotal role in leading the Glasgow Royal Infirmary (GRI) through the extremely difficult challenge of managing Covid. Aleks has helped every clinician in the North Sector during the Covid pandemic, providing advice and guidance throughout, running every Incident Management team meeting and being at the end of a phone for every challenging decision. She is always kind and helpful even in difficult circumstances. The GRI would not have managed through the Covid pandemic without her help, leadership and guidance.

Julie Graham, SCN Ward 56, which is usually the Gynaecology elective and emergency ward, but during COVID has been used as a COVID hub ward and medical contact ward. Julie has led her team through a hugely challenging year and most recently some very challenging weeks.
Julie’s approach has been one of ‘can do’, whilst keeping patient safety and the wellbeing of her team at the forefront. For the GRI site having Julie and her team approach every challenge with this attitude has made the difficult operational ward moves much easier.

During the second wave of the COVID pandemic a team of redeployed Rotational Physiotherapists came together to provide a Physiotherapy Service to the COVID High Dependency Unit (CHDU). This was not only to assist in providing early rehabilitation but also to support nursing staff with oxygen delivery and nursing roles.
The objectives were to assist nursing staff with basic nursing care, allowing breaks from PPE, to provide advice and knowledge of oxygen and CPAP therapy to nursing staff that had not been exposed to this before as well as setting out to achieve the Physiotherapy goal of providing early rehabilitation for patients.

This especially young team of individuals has offered an invaluable service to our organisation throughout the pandemic. They politely and eloquently handled our front door for the general public at a very challenging time. Patients received their personal belongings that provided them with contact with their families and loved ones. They were remarkable young folk with a constant smile and support to our stretched teams on the ground and provided a significant contribution to patient centred care, consistently demonstrating an exemplary focus on our patients and ensuring they are treated with care, compassion, dignity and respect in receiving safe and high quality care.

Dr Ross Shearer has been awarded the ‘Wellbeing Champion’ Award in the North Sector in recognition of the significant contribution he has made to the health and wellbeing of our staff, in taking action to ensure we are as healthy and as well as can be, and increasing our resilience as a workforce.
Throughout the pandemic Ross has provided psychological support and advice to colleagues across NHSGGC. Ross attended various R&R hubs across NHSGGC’s sites offering psychological support and advice, and offered sessions over the phone and in small staff groups.
The South Sector would like to take the opportunity to thank all our colleagues for the outstanding work and contribution they have all made to patient care during the most difficult period we have ever experienced. This award is to put on record that all colleagues and teams across the South Sector came together to help support and assist each other to meet the challenges and deliver the best care for our patients during a global pandemic.

Terri has assisted a number of teams and individuals across the South Sector since joining the sector.
The appreciation and understanding of the work of OD has risen as Team relationships/Service developments and Organisational change projects have all benefited from her innovative approaches to resolving issues & concerns. Terri was also integral to the development and installation of the R&R hubs within South Sector Hospitals ensuring they were staffed and resourced during the most difficult Covid periods.

Together, the Chief Residents have played a vital role in facilitating good communication of the important issues within the department. They have organised and lead upon some key initiatives including:
In addition the Chief Residents have lead on a comprehensive Wellbeing QI programme throughout the past 18 months. Numerous ‘events’ have been run all with the aim of boosting morale and teamwork in the trainees.

The QISS team have developed a strategy for raising the profile of Quality Improvement (QI) in the South Sector. Despite the challenges of the pandemic, all involved have endeavoured to mentor interested staff members as they undertake QI projects in our clinical areas. In the past eighteen months, 21 projects have received input from the team.
The Team have launched a share-point website as a resource for all south sector staff. This provides QI information and toolkits, links to our mentoring services and signposting to training opportunities.

Mary managed the Give and Go project allowing relatives, who were unable to see patients on the wards, to ensure their loved ones received some home comforts during their stay. Mary was also led on the return of the Volunteer teams to the Hospital sites ensuring individuals where supported and assisted during the initial stages of the restart addressing and answering their individual concerns.
All staff at every level within Virology have performed exceptionally well under extreme and sustained pressure over the course of the pandemic, coming together to not only design, establish and commission a brand new laboratory, but to enhance the existing NHS Lab in order to upscale and maintain large volume testing for COVID-19. This includes the clinical liaison and advice provided both internally and at the national level. A large number of staff volunteered to work excess hours and extended working hours in order to ensure that all could access timely and effective diagnostic testing and advice.

Bernadette was the driving force behind the rapid upscaling of current COVID-19 testing capacity and the formation of the West Regional Hub for COVID testing. Working tirelessly for months over the course of the pandemic, often on her days off to increase our COVID testing capacity, Bernadette grew capacity from 300 samples to 3,330 samples per day. This included inputting to designing and commissioning a bespoke Laboratory for large volume COVID testing.
Her ability to maintain her composure under high stress and during periods of frenetic activity was second to none and instrumental to achieving something in 3 months, which would otherwise take 18 – 24 months.

When COVID-19 arrived, as the Head of Service, Ted took on so much more. He galvanised the Gartnavel General Team to use their innovative technical skills to repurpose anaesthetic machines into ventilators. He worked with the Louisa Jordan Hospital Team to medically equip the facility and make it fit for purpose. His leadership qualities, knowledge and expertise and can do attitude was recognised by the Scottish Government and as a result he was asked to direct the NHS Scotland project that was to result in the repurposing of approximately 200 anaesthetic machines into ventilators.

The department successfully established the UK’s first routine Single Photon Emission Computed Tomography (SPECT) Coronary Flow Reserve (CFR) service. The service was set-up using a state of the art Solid State Gamma Camera (the first of its type in Scotland), and was done in collaboration with both GE Healthcare and Cardiology colleagues in Italy. This new service is now available to Cardiology referrers throughout the West coast of Scotland, from Dumfries and Galloway to the Western Isles. Establishing a SPECT CFR service has been critical in giving clinicians in NHSGGC an additional routinely available tool to aid with the assessment of diagnostically complex cardiac patients.
This service entered the pandemic in a state of upheaval following a difficult review process and requiring the introduction of a new structure. They maintained support to customers throughout the pandemic and did not suspend or reduce a single package of support. Dealt with higher demand of community and hospital referrals. An anonymised customer survey indicated positive perceptions of the service.
The District Nursing service continued to visit vulnerable patients often the only service received by patients and families at the beginning of the pandemic. They provided emotional, psychological and spiritual support to patients and their families allowing care to be provided in the patient’s place of choosing. They demonstrated effective team working, resilience, flexibility and creativity to ensure safe, effective person centred care to meet the increased demands on the service.

Kerry and Michelle were redeployed to support the setting up and running of the Kirkintilloch Covid Assessment Centre, including providing clinical induction to local GPs and providing a significant proportion of clinical shifts to assess extremely ill and deteriorating Covid patients during the first wave. They demonstrated extreme skill in developing safe and effective practices and procedures for the CAC. They provided enhanced clinical support to Care Home residents when homes were in active Covid outbreak during the first wave. Feedback from Care Home staff, GP’s and families is this this service was of significant value.

Vandrew joined the HSCP in March 2020 and quickly made a positive contribution. She ensured that business support teams were mobilised effectively to support front line staff during these challenging times by supporting the set-up of the PPE hub, setting up a team to support the covid vaccination programme/testing, undertaking risk assessments and working with council colleagues across our buildings and putting in place arrangements to ensure these were safe places for staff to continue to deliver critical services

Working in partnership the mental health services and health visitors provided information sessions and access to an enhanced range of treatment options for new mothers to support children’s wellbeing. They developed a project plan capturing a range of services that support mothers experiencing mild to moderate mental health difficulties in the post-natal period. They provided new mothers access to group work, access to 1-1 sessions using tools to support mental health and wellbeing through universal services.
The Public Dental Service provides care to children who have additional needs, medical conditions and extensive decay and who are at risk of high levels of associated pain. In order to alleviate this dental pain and discomfort, historically the best available option has been extractions under general aesthetic. However, due to the Covid pandemic and restrictions on access to theatre the team took the opportunity to look at innovative and alternative models of care that could improve child health and wellbeing allowing them to avoid a GA pathway and receive less invasive and more holistic dental care in a timely manner, in a local dental setting.

During the lockdown period the group supported the development and distribution of regular public health information through a monthly newsletter. The publication highlighted the spread and impact of Covid within and across East Dunbartonshire, promoting the community immunisation clinics and advised where to access the most up to date data and information towards keeping their families safe and well. The group developed a series of public health ‘Biteable’ social media videos; detailing crucial information for the local community, including changes and how to access General Practice.
From the beginning of the pandemic our commissioning team started daily contact with care homes.
When outbreaks started, it became clear they needed additional support. Many found themselves short of staff as they too became sick with the virus or were self-isolating/shielding.
Having identified the growing problem, the HSCP quickly mobilised and the Care Home Assurance team was created.
The team was made up of staff from a range of services including commissioning, nursing, rehab, social work and older adult’s mental health. The aim was to provide support to all 13 care homes in East Renfrewshire to help control any COVID-19 outbreaks, ensure preventative measures were in place and to bring health and social care services together to best support each home.

Jennifer Clark’s role encompasses responsibility for premises, lead role for Health and Safety, updating and maintaining the Business Continuity in addition to having direct line management for nine members of staff.
Jennifer started the role in January 2020 and within two months the HSCP had moved to an emergency footing as the partnership responded to the pandemic.
She has worked closely with staff members to build and develop team work across the teams she has responsibility for, creating a “can do” culture where staff are keen to work together and engage in new approaches to support the partnership to achieve its key objectives.

Mairi-Clare manages over 100 members of staff. This includes the entire Business Support output for the HSCP, Facilities Management for Eastwood and Barrhead Health and Care Centres, HSCP Change Programme (now Recovery and Renewal), Information and Systems, Governance and the DMT Personal Assistants.
Mairi-Clare is the backbone of the HSCP, she helps everything behind the scenes work together and empowers her teams to deliver their own work to a high standard. While her normal role makes her invaluable to the HSCP, she has also been responsible for leading significant projects during the pandemic.

During the second lockdown the HSCP Children & Families service was worried about the young people known to their service, as they were spending lots of time indoors and had disengaged from learning, activities, clubs and their communities.
They wanted to deliver a project that would provide young people of all ages the opportunity to try new skills outside of their home, build confidence, encourage them to socialise again and to help them feel part of their community.
As a result the Enrichment Activity Programme was devised. The team went the extra mile at every stage of this project. They provided an enriching experience for the young people they support.
This significant project needed to be set up rapidly through a collaboration of work by all of the eHealth team (Operations, Strategy and Programmes, Information Management and Health Records). Operations and telecommunications were pivotal in setting up a new call centre with all of the appropriate telephony and IT kit. The set-up had to be done in a way that utilised existing clinical systems capability to support the newly defined pathways – ensuring those patients requiring tests, admitted or remotely monitored were captured and managed accordingly. A completely new patient booking system which enabled patients to contact the Centre to change appointments or to email queries relating to the vaccine, where appropriate.
The focus of this project was to rapidly accelerate the set-up, management and data recording of Virtual Patient Appointments for acute and primary care. This allowed optimisation of virtual patient appointment management including the delivery of
This project was critical to the Board’s ability to maintain outpatient and GP appointments in response to the pandemic.
This programme of work involved all eHealth teams including, Strategy and Programmes, Operations, Information Management, Information Governance and Health Records staff.
The eHealth team was pivotal in working with the NHSGGC Vaccination team to put the technology, telephony, reporting and for recruiting, defining working processes and training the contact centre staffing required to support the Board Covid Vaccination Programme.
eHealth and the wider GGC vaccination team worked with NES to develop the Vaccination Management Tool which was rolled out across NHSScotland to record vaccinations across all settings.
eHealth teams also supported the set-up of the vaccination centres for staff and the public without which the Board would not have been able to start the vaccination programme as swiftly as it did and to maintain it as efficiently as it is now doing.
This project involved the rapid Introduction of Patient Flow Hubs to direct patients to appropriate services to reduce unnecessary pressures on Emergency Department attendances. eHealth were key stakeholders in the redesign of urgent care pathways to direct patients to the appropriate service where this is clinically appropriate and safe to do so. A key element of the change was the implementation of a Flow Navigation Centre (Hub) to support the appropriate flow of patients.
Health Records played a central role in coordinating operational activity to ensure patients were booked in a timely manner. The collaboration and flexibility demonstrated by eHealth teams cannot be understated and formed a key part of the Board’s response to improving unscheduled care.
The Inverclyde Royal Hospital Estates Team were faced with replacing non-compliant switchgear components to safeguard the resilience of the main hospital electrical supply to both critical and non-critical services on the site. Ross Campbell, Site Operational Estates Manager, and his team embarked on an extensive and very difficult programme of modernising electrical switchboard components. This project had to be carried out whilst the hospital was at full patient capacity, and at the height of the pandemic in 2020 which added another level of complexity. The team have shown a huge commitment to their roles and were acutely aware of the impact that would be experienced if the work was not carried out meticulously.

In a department which has endured significant challenges and change over the last couple of years, including through the COVID Pandemic, Mark has continually demonstrated his significant value to the Estates Team and has played a pivotal role in the evolution of the Estates department, who are widely respected throughout the campus for their committed, caring and professional approach.
Mark’s work ethos and approach to his day to day duties and responsibilities are exemplary and he sets such high standards in all aspects of his role, which has had a positive impact across the Estates Team.

Billy displayed a level of leadership across Soft FM services during the COVID Pandemic, which was pivotal in ensuring these key services were supported to meet the demand and challenges faced, often changing on an hourly basis.
Over the last 18 months, Billy has developed an approach for his team, which has seen positive improvements across the full service, whether recruiting staff to support the increased cleaning requirement, sourcing cleaning materials, ensuring updated guidance was implemented and perhaps most importantly ensuring staff on the front line felt supported by their management teams.
The overall approach and impact of Billy’s leadership has seen improved staff morale.

Tom Fulton has always used both his 30+ years’ experience and knowledge of the site to ensure best value with local projects and is considered an active participator in the development of the site and future investment.
Tom has also assisted and been very proactive in the development of the Glasgow Royal Infirmary Museum project which will allow both staff and patients to access the history of the historical site for now and the future.
Tom who will shortly retire, is an ambassador of Glasgow Royal Infirmary and has always put patient needs and environment at the core of everything he does.

During the early stages of the Pandemic, the workload within the Cowlairs Decontamination Unit significantly reduced. All staff were offered the opportunity to volunteer to be reassigned to support other services, principally at Hillington Laundry where there was significant pressure on provision of services.
These staff volunteered to be reassigned, taking on the challenge of working in a different area and a different service at Hillington laundry, and assisting with the increased demand. This had a significant impact on the service, proving much needed support in the provision on laundry for patients and also scrub suits for relevant departments.
Since the start of the pandemic most services have experienced additional demands and pressures while also coping with the sudden shift in March 2020 from business as usual to living and working safely in a Covid world while still providing business critical services.
During this time Payroll Services has been one of the hidden hero services for the Health Board. Workloads across the service increased significantly, Payroll teams have been required to process several thousand additional temporary and permanent staff arrangements, over 6,000 new starts in one month. In addition there have been multiple pay awards, new terms and conditions, new service areas requiring support like vaccination services and the complexity of the Covid Recognition Payments, all of which added to the Payroll Services burden.

Fiona has been instrumental in the costings for the Covid-19 costs around Test & Protect, Vaccinations and Public Health. This has involved a lot of extra work and Fiona has showed great dedication and commitment throughout the pandemic. She has been the key link with all the corporate departments and her assistances has been invaluable to the Finance Team and the Corporate areas she deals with.
She has also been a great support to all the senior management team as there has been transition between roles. Fiona takes a very balanced view on issues and always considers both sides of an argument.

Elaine has been the Senior Management Accountant in the Regional team through some particularly challenging times.
There have been many difficulties within the team which Elaine dealt with this admirably switching tasks between team members and engaging with her Principal Finance Manager and Head of Finance.
During the lockdowns and covid period Elaine encouraged her staff to meet weekly on a Friday afternoon for some downtime to help and encourage wellbeing within her team. These times seem to have been thoroughly enjoyed by her team.

Value management is a national improvement collaborative that aims to test and spread an innovative model that supports clinical, care and finance teams to apply quality improvement methods with combined quality and cost data at team level to deliver improved patient outcomes, experience and value.
The collaborative, led by Healthcare Improvement Scotland’s ihub, working in partnership with NHS Education for Scotland (NES) and the Institute for Healthcare Improvement (IHI) launched in November 2019.
As part of the value management (VM) multidisciplinary team Alan spent a lot of time designing a process to quickly capture the required finance data for the VM box score.
The Occupational Health Nursing Team led a significant piece of work in supporting all our staffs’ health and wellbeing through the last 19 months. Not only have the team continued to provide support on a personal basis to individuals and managing attendance they have also and were heavily involved in the early days supporting the Vaccination Programme and Fit Testing and providing advice and support to the staff for risk assessments. They continue to provide ongoing support to our staff with Long-Covid.

Allan has shown leadership and commitment in coordinating and supporting the Fit Test Programme for NHS Greater Glasgow and Clyde (NHSGGC). He has gained significant knowledge in the field and has provided advice and support through not only the Health and Safety Team but to Managers and Services throughout the Board.

Nareen as our Depute Director of Human Resources & Organisational Development has not only supported our overarching one team approach but has shown true leadership in supporting all of our teams to deliver our current services but also a range of new services to support COVID over the past year.

Steven Munce, Neil McGhie and Morag Kinnear along with others in recruitment and other teams helped set up the Test and Protect Team from scratch. Not only recruiting everyone but ensuring all the rosters and the systems were in place to support Public Health.

The Organisational Development Team initially helped to set up the R&R Hubs across all the main sites which included everything from organising the teas and coffees, organising furniture to ensuring that all the relevant staff support was put in place and they continue to support the Programme overall.
Inverclyde HSCP Care and Support at Home service provides personal care and housing support to adults living at home, with the majority of service users being older people. The service works over seven days and includes Community Alarm and Technology Enabled Care which operates on a 24 hour basis.
Care and Support at Home staff continued to provide essential service to all service users from the start of the pandemic and at a time when there was little known about the situation or how long it would continue. Every member of staff knows how essential the service is for people at home and accepted the need to continue as normal in the face of this crisis.

When the Covid-19 pandemic arrived, Community Mental Health Services (CMHS) had to reconfigure to a critical Mental Health Hub. The purpose of this was to ensure reactive capacity for community urgency and prioritised scheduled service delivery in an accessible and sustainable way for more than two thousand service users.
Susan was pivotal in identifying and outlining the essential service areas at the initial outset of the pandemic. This led into the necessary conversations and planning with other CMHS team leads to establish the strategy, operationalise and ensure sustainability of the priority elements.

Kate began her career in social work in February 2008. Her capacity to form strong and lasting relationships was a hallmark of her as a person and a professional. She has always appeared calm and serene and had been able to instil this in colleagues earning immediate respect of all who worked with her. In response to unprecedented recruitment challenges in Inverclyde over the past 18 months and in recognition of the increasing challenges for our new social workers, Kate established a local academy. This has helped to equip our newly qualified staff to the best possible standard as they embark on their career.
During the pandemic she displayed all of the qualities and attributes that are required by a strong and compassionate leader. Properly supported and nurtured staff in Inverclyde were able to maintain a high level of contact with service users throughout the pandemic. Sadly, our friend and colleague Kate Christmas passed away on the 14th of July this year after a very brief illness.

Since the onset of COVID-19 in March 2020 the team reviewed their practices and ways of working, moving to more streamlined and digital processes. As part of this process they have taken forward and successfully piloted for Inverclyde HSCP, video consultation calls via the NHS Near Me / Attend Anywhere web-based platform. Their Attend Anywhere model focuses on people and processes, not just technology.
People have been seen more promptly and waiting times minimised. They have been more effective in reaching vulnerable people for example those with mental health issues and mobility issues and for people with a history of non-engagement with services.
At the height of the pandemic the number of critical care beds increased 4 fold. Working collaboratively across sites the critical care team rapidly upskilled and trained pharmacy nursing and medical staff, highlighted and monitored medicines shortages and risks, reviewed their clinical service provision over 7 days providing leadership and expertise locally and nationally. The core team was supplemented by staff from a number of other areas who volunteered to be redeployed to support critical care either in direct patient care or in supporting roles.
Vaccine delivery required a new way of working that crossed different teams and settings to provide pharmaceutical expertise, product stock management and delivery of vaccine to staff, care homes and community vaccination clinics. This was a true multi-disciplinary approach from pharmacists, pharmacy technicians, pharmacy support workers and administrative staff from across all areas of our service including, Pharmacy Public Health, Pharmacy Distribution Centre, Regional Quality Assurance and prescribing support

Denise is a Care at Home Pharmacy Technician who always shows care and compassion when dealing with patients, she goes above and beyond to help patients at all times. She is an integral part of the team. She liaised closely with the GP practices to ensure communication was maintained. She spent time supporting other team members, promoting their mental wellbeing and ensuring support available when people were struggling with workload. Denise is also the HSCP’s cold chain champion and had an essential role in the opening and running of 3 COVID vaccination clinics whilst maintaining her substantive post’s workload.

Sam is an inspirational leader of the Research & Innovation Clinical Trials Pharmacy Service. Her leadership skills have been outstanding over the last 18 months in dealing and responding to the impact of COVID-19. Sam has led the team setting up COVID-19 clinical trials in response to every stage of the pandemic; from community-based projects to researching suitable treatments for acutely ill patients in ITU to establishing crucial vaccine clinical trials. These studies were set up at a faster pace than ever seen before, which may not have been possible without the leadership, hard work, extra hours, expertise, experience and absolute determination.

A prototype visualisation of medication history for patients attend epilepsy and difficult asthma clinics. It allows clinicians in a hospital setting to see the medication that patients have been supplied with in the community as an objective measure of adherence based on national prescription data. Generally, patient self-reported adherence to medicine is inaccurate and healthcare professionals tend to overestimate patient’s adherence. Improving adherence contributes to better health outcomes, reduces health system costs and improves the lives of people with chronic diseases. The project also provides educational resources and advice on how to use motivational interviewing to facilitate effective communication about medication adherence.

Pharmacy Services do not use volunteers, however the Director of Pharmacy and Pharmacy Services Partnership Forum wished to recognise the contribution of all staff during the pandemic. The goodwill and exemplary professional behaviour exhibited by all staff ensured care for patients was not interrupted and that staff supported each other during these very difficult months.
The HP Nurses have played a pivotal role working across health protection and the test and protect service throughout the pandemic. They have worked tirelessly providing expert advice to care homes, NHS colleagues, HSCPs and the public, to name but a few on all aspects of Covid – from managing clusters and outbreaks to contact tracing, vaccination and everything in between.

Janet Campbell manages the NHS staff Covid testing service which has been running since the start of the pandemic. Her hard work, commitment and flexibility means that this testing service, based in the West ACH is available seven days a week.

Employed 19 team leaders and two service managers, the majority of whom are from the private sector and helped create a vision and a goal of the Test and Protect service within GGC. In a short period of time created a service consisting of approximately 200 staff with a family feel – all of whom are on fixed term contracts and had them working to every NHS value. Has shown an open door policy and has been there for each tracer, team lead and service manager when they are at their lowest, even picking up the phone to contact trace herself.

The weekly staff forum was created to provide stronger communication between contact tracing staff and the leadership team. It provides a ‘one stop shop’ to improve communication across the Test and Protect service as key information was scattered across separate team channels and chats and difficult to find. Missing these important pieces of information, e.g. changes in policies and procedures, could negatively impact on the outcome of a call to a patient. The forum empowers contact tracers to bring their ideas and vision to improve the service.

The R&R hubs provided a safe & secure non clinical environment for staff to rest & recuperate during the height of the pandemic. This service was open 24/7 for the first 6-7 months. The public health staff provided a listening ear and were able to signpost staff to support services as required or requested. They also provided staff with the opportunity to engage in activities that supported good mental & physical health. Relationships with staff were built on trust, confidentiality, friendship & respect & this resource was very well received.
During recent uncertain and stressful times, Renal Transplant nurses were meticulous in their care of patients who were isolated from their families in hospital. The Renal Transplant Team went on to perform one hundred transplants between March 2020 and the start of December 2020, including twenty–five living donor transplants, with no cases of nosocomial coronavirus infection despite the highest prevalence of COVID-19 infection in Scotland in both the Glasgow community and the QEUH. These achievements all took place in the context of huge pressure on the team as a result of sickness absences, including cases of COVID-19 amongst unit nurses, COVID-19 related absence due to self-isolation and childcare.

During the initial outbreak of Covid-19 John consistently worked above and beyond the remit of his role within the Dialysis Unit at Inverclyde Royal Infirmary. Throughout the outbreak he not only performed his role to the highest standard, but consistently provided a reliable and supportive influence towards his colleagues at a complex and challenging time.
Over and above this John supported patients out with the unit, including those who were either Covid-19 positive or who were shielding without any family support. In practice, this comprised grocery shopping, collecting prescriptions, assisting with documentation and any other requirement patients had including helping to look after one patient’s beloved dog.

In response to the Covid-19 pandemic and to allow more patients to remain on-site at Gartnavel General Hospital in the absence of on-site critical care, Judith quickly set up and established the Beatson High Acuity Unit (HAU) and Critical Care Service as a safe and effective service for unwell Haematology and Oncology patients being treated at the Beatson West of Scotland Cancer Centre.
The outcome of Judith’s outstanding leadership and the actions of her team resulted in providing a higher level of patient care at an unprecedented time of concern.

In order to reduce their risk of coming into contact with patients with Covid-19 and to ensure that patients remained outside the main hospital building at Glasgow Royal Infirmary, a joint Trauma Assessment Service was set up in collaboration with Orthopaedics using an outpatient facility in the Gatehouse building. A joint trauma assessment service had been considered for a long time, however it took the emergence of COVID-19 for the Plastics Trauma See and Treat Service to be set up and become operational in a matter of days. This was down to outstanding leadership, collaboration and first class team-based working.
Health and Social care should enable people to live the lives they choose in the best way possible.
Care at Home has represented HSCP’s vision in the most extraordinary way over the past 18 months, operating tirelessly to support vulnerable people against the uncertainty of a pandemic.
This team wouldn’t class themselves as special if you were to ask, they would simply just tell you that they are doing the job they love. That’s what makes them special.

Patrick or ‘Pat’ as he is well known is a ‘one-man team’. He does his job without any qualms and complaints. I have never seen him saying no to anyone, even if there is something that is beyond his role he would happily agree to find a solution. He treats professionals, patients, carers, and members of the public with the same regard and respect.
Everyone who enters Renfrew Health & Social Work Centre knows ‘friendly Pat’. He is a star who needs to be acknowledged for altruistic efforts!

Madeline has led the District Nursing team through one of the most challenging and demanding times within nursing. Over the past 11 months, Madeline has been the only Team Lead for all of the district nurses within Renfrewshire and she has demonstrated tenacity and resilience in the face of adversity.
Madeline is dedicated to the district nursing service and passionate about ensuring that nurses are supported to deliver person centered care.
She is the epitome of resilience and has the ability to manage challenging situations with care and compassion.

In a year that has been challenging for everyone, Renfrewshire Learning Disabilities Service (RLDS) worked hard to find alternative ways to connect with individuals and provide support for those who access the service.
Staff tackled the challenges to make sure that our supported people had the opportunity to try new activities and stay connected in a meaningful way.
Which in turn, supported their parents and carers to have valuable respite from their caring responsibilities during this unprecedented time.

Both Jim and Anne deliver food from the foodbanks throughout Renfrewshire to households. Jim also picks up medication from Pharmacies.
They truly are selfless, caring, non-judgemental individuals with a strong sense of community who give so much of their time and energy.
There have been many times when they have put their own lives on hold to help those in need and this should be rewarded in some way.
At a time when others were staying at home, they were out in the communities helping those in need despite a global pandemic!

This group of people responded instantly and continued to input into a crisis situation within one of the Renfrewshire care homes, which unfortunately suffered a significant COVID-19 outbreak affecting almost 80% of its staff and over 90% of their residents.
This was very much a crisis situation with the home requiring immediate and sustained support to ensure that the residents whom many were symptomatically unwell due to COVID continued to receive the best care.
All worked to provide direct patient care and to support our care home colleagues which without the support of this group of staff the residents would have been all at risk.
Connect ED is the specialist eating disorders team in CAMHS. The team support, deliver and evaluate evidence based treatment for young people suffering from eating disorders in GGC.
Throughout the pandemic the team worked tirelessly to find ways to provide treatment for families using digital resources, adapting well to this new way of working. The team continued to deliver evidence based treatments and developed groups aimed to support the increased number of referrals. Altogether it has shown that CAMHS works well together and pulls on all the skills and expertise within the team.
Tier 4 admin hub were put together a number of years ago when staff from different teams across Specialist Children’s Services came together to form the Tier 4 Hub.
Over the last year the team demonstrated commitment to their roles. Staff are all very caring towards each other and will often check up on each other even after work if it is felt someone needs it. It feels a very safe place to work as staff trust each other.
This team plays a vital role in supporting all the teams at tier 4 and have done so throughout Covid-19 – they have pulled out all the stops to support everyone and have looked after each other.

Jacqui Ely joined the team at Skye House two years ago as a Ward Clerk Since that time Jacqui has excelled in what she does in the ward with both staff and patients. Jacqui is very creative and has transformed the ward with pictures and staff boards and has made the ward a much more welcoming place for young people and their visitors. We have had very positive feedback from patients and their families about how welcoming Jacqui makes them feel when they come to the ward and ensures they have what they need and is a friendly and extremely helpful person for those who come to the ward in an often distressed and emotional state.

Paediatric Psychology delivers psychological assessment and therapies to children, young people and families under the care of the RHC experiencing psychological/mental health difficulties as a result of their medical condition or treatment.
With the onset of COVID-19, the Paediatric Psychology team recognising the considerable psychological strain the COVID pandemic placed on staff across the whole hospital, the team gained support from SCS management to divert some of their time to staff support. Staff were supported to manage the stress and distress of their jobs and many fed back that the tea break talks had been invaluable in enabling them to continue delivering high quality care to their patients.
Care Homes faced immense pressure during the pandemic, always striving to strike the right balance of keeping people safe while supporting them to live fulfilling lives through person centred care. In response, the teams rapidly adapted their practices, working tirelessly to accommodate new guidelines and policies in a constantly evolving situation. Together they learned, shared and supported each other through a range of emotions – sadness, loss, anxiety and fear of the unknown – but at all times their primary focus was keeping safe the vulnerable residents in their care.
They embraced technology as a way to stimulate and promote the wellbeing of residents, creating a Facebook page, WhatsApp groups, composing newsletters and using Zoom to ensure regular contact with families.
Care at Home services are integral to the HSCP’s commitment to support people to live well independently in their communities for as long as possible. So when the COVID-19 pandemic took hold the Team’s biggest concern was the equally virulent spread of another scourge for their shielding clients – loneliness.
Cut off from trusted carers and neighbours, their isolation inevitably took its toll on their mental health. But thankfully, they would soon find that they are not alone.
The response from the Home Care, Sheltered Housing and Community Alarm teams was a collaborative approach, working with partner agencies and family members to ensure that services could be targeted to those most in need.

Resilience and resourcefulness, care and compassion. Such qualities were needed more than ever during this turbulent Covid era and Denise Ferguson displayed them all with unstinting commitment to supporting her patients and colleagues alike.
Her quick response in the early stages of lockdown ensured that local teams had the resources required to work remotely and maintain strong communication links with GP Practices.
In addition to her role as a Care at Home Pharmacy Technician, Denise played an integral part in setting up and running three Covid vaccination clinics in West Dunbartonshire, ensuring that the “cold chain” protocols for the vaccines were maintained.

It’s during tough times when great leaders are defined and Heather Caughey undoubtedly rose to the challenges posed to her MSK Physiotherapy service during the pandemic.
Accepting overall responsibility for establishing a functioning face-to-face MSK service at the Louisa Jordan Hospital, she identified, co-ordinated and monitored all of the practical arrangements. This included selecting and moving staff, equipment, clinical notes and students to the newly set up facility.
She also co-ordinated the de-commissioning of the service in a very short time frame when the Hospital closed.
Without exception, those redeployed to work under her leadership in the Louisa Jordan found it a rewarding and enjoyable experience.

For a service that epitomises hands-on care, the sudden onset of social distancing restrictions posed huge challenges for the MSK Physiotherapy Team.
A positive “can do” attitude and willingness to learn new skills was at the heart of the team’s swift and innovative response, embracing technology to create new opportunities to deliver modern quality care.
Digital capabilities were developed, not only for patient consultations but also a wide range of activities including the creation of a Covid Clinical Pathway to share knowledge and wellbeing resources.
These “best practice” elements now feature as part of a comprehensive digital strategy employed across the wider NHS community.
Throughout the past 18 months the Royal Alexandra Hospital (RAH) Community Midwifery Unit have worked exceptionally hard to provide excellent care to mums, babies and new families during the pandemic. Adapting to closures of their department and supporting other departments not only within the RAH maternity unit but the other maternity sites across NHSGGC as well. The team acted and adapted quickly to working in unfamiliar areas, to new pathways and processes and making full use of new technology via video/telephone appointments which allow them to keep in contact with their patients and families.
The Acute Paediatric Physiotherapy service within the Royal Hospital for Children (RHC) responded with initiative, efficiency and professionalism as the Covid-19 pandemic unfolded. They quickly shifted working practice for outpatient services to virtual and telephone using near-me, supported MDT clinics using near-me, liaised with and supported adult colleagues, set up training for all Paediatric staff on proning, manual handling and adult respiratory skills, and ran practical sessions on donning and doffing PPE to other AHP colleagues within RHC.
The team also prepared and delivered online training for colleagues across Scotland and the RHC has been recognised as one of the leading sites in virtual student placements and the benefits of peer supported learning throughout the Physiotherapy profession.

Debbie Harrison is in the team looking after children with malignant haematological and oncological diseases and children undergoing the Stem cell transplant process.
As a caring and compassionate nurse who works hard to ensure that children with leukaemia receive the best care possible, Debbie has maintained a positive outlook and supported and encouraged others despite the department going through touch changes and challenges over the last 4-5 years. Debbie has faced challenges from the children’s hospital to the adult hospital, staffing shortages and the added burden of caring for very immune compromised patients through the pandemic with a smile and always has an encouraging word for others.
Claire Rowan is a Practice Development Midwife who created and rolled out an induction programme for Newly Qualified Midwifes (NQMs) that was adapted specifically for COVID restrictions, and managed to deliver the whole programme despite COVID and all of the restrictions and pressures that came along with it. Moving the programme from what was initially face-to-face education in the QEUH Teaching and Learning Centre, to a hybrid of small learning groups and flexible e-learning in 2020 and 2021.
Instead of attending 75 hours of lectures, NQMs now attend 24 hours of interactive education, and complete a comprehensive e-learning list.

Through the COVID pandemic Jennifer Johansson took notice that midwives were experiencing change at a significant pace and facing incredible challenges both within and outwith their working environment, and decided to do something about it. Jennifer commenced a project in October 2020 to enable the senior labour ward staff to facilitate time for staff to concentrate on their wellbeing and wellness at work. The aim was that a minimum of 50% of midwives on shift would receive a 10 minute wellness break in a designated wellness room in the labour ward. The outcome was achieved with well over 50% of staff benefiting from a wellness break and excellent feedback from staff using the facility.

A new patient centred ‘Outpatient Induction of Labour’ service was introduced during the pandemic, with the aim to reduce hospital admissions, reduce the caesarean section and assisted birth rate and provide women with an innovative safe method of inducing labour and then safely go home to be with their families and return the next day.
This was a very challenging service to set up initially but with head-strong determination and unbelievable team work and motivation the QEUH Ward 48 team are now seeing the results. The process has had a 96% success rate and women are able to transfer to labour wards to have their waters broken without the requirement for an inpatient stay, without requiring drugs and with minimal discomfort.

Michelle was approached at the beginning of the Pandemic with a request to set up a robust admin system to book in Covid vaccine appointments for Medical, Nursing and Clinical Staff members in the Women’s and Children’s (W&Cs) Directorate. Michelle embraced this request, learning the new technology and setting up a Microsoft TEAMs page with an excel file recording all staff bookings. She worked from home outwith her normal working hours, at weekends and late into the evenings to book in staff to the appointments as they became available as well as phoning staff members advising them of their appointments whilst answering any queries they had.

Paediatric Consultant Dr Morag Wilson along with Coral Brady, Seona Hamilton, Melville Dixon, Graham Bell and Geetika Kumar at the Royal Hospital for Children have worked to develop an app for parents and carers that provides a wealth of information for children’s health.
The app and accompanying webpage not only give advice about how to access care for different situations, but also what to expect when visiting the Royal Hospital for Children (RHC) and information on common childhood issues such as earache, fevers and temperatures and coughs and colds.
The app was developed with parents, carers and children in mind, understanding that it can be very stressful when a child is unwell.

Conor Doherty has been awarded the ‘Directors Award’ in the Women and Children’s Directorate in recognition of his exemplary performance and behaviours, playing a pivotal part in meeting our goals, driving our positive culture and moving the Directorate forward safely through Covid.
Throughout the pandemic Conor has played the lead role in ensuring that the Royal Hospital for Children (RHC) is in a strong position to deal with the pandemic whilst maintaining a safe clinical environment for the children, families and staff. Conor has taken on a key leadership role, keeping the whole clinical team informed of the most recent developments in epidemiology and national standards such as with PPE and infection control measures throughout.
The team, department, service or function that has been judged to have worked together as a team and made the most significant contribution to quality of care, population health and care, service delivery or staff wellbeing likely under significant pressure or difficult circumstances.
Any member of staff who has stood out as an exemplar of care giving, service delivery or who has made a major difference for colleagues around them or the delivery of a key objective for their department or wider NHSGGC/HSCP.
Any member of staff who has demonstrated outstanding leadership, positive values and behaviours and/or inspired others in a particularly challenging situation, or for the respect they get from others through the day to day difference they make for those around them as a leader.
Any member of staff can demonstrate leadership, not just those who formally manage people.
To recognise any individual, team or department responsible for developing and implementing an innovative service, method, technology or process that has made a significant difference to quality of care, wider population health or care, service delivery or to the wellbeing of our own staff or to the efficient use our resources.
To recognise an individual or team of individuals who have volunteered significant time and effort to the benefit of our patients, service users or staff and made selfless contribution perhaps under difficult personal circumstances.
Our prestigious Excellence Awards are for individual members of staff or teams, or projects that have identified ways to deliver improvements that benefit our patients, service users, colleagues or NHSGGC. The awards consist of eight categories, which you can find out more about in the Nominees list below.
The awards were presented at the virtual Celebrating Success Awards held on 23rd February 2022 which you can watch on this page further below.
You can find out more about each of the overall winners via the video links below, and read about the nominees who were shortlisted.
Congratulations to all the winners and nominees.
The awards were presented at the virtual Celebrating Success Awards held on 23rd February 2022, hosted by Professor Jason Leitch CBE, National Clinical Director.
Our dedicated teams and individuals are nominated for NHSGGC Excellence Awards by patients, visitors and staff. All of our staff have gone above and beyond in the past 18 months and we asked to hear about your experience of outstanding care and for your nominations.
The nominees in each of the categories, are listed below:
This award recognises staff who provide and contribute towards incredible patient care improving everyday practices across NHSGGC.
At the start of the pandemic, it became clear that those who became very ill with Covid need a place where they could be seen and assessed safely and away from non-Covid patients.
Our Community Assessment Centres were created. This significant project required input from all of the eHealth teams to ensure the centres had all the necessary telephony and IT kit. They also needed to be set up very quickly.
eHealth teams responded to the needs of the service, working above and beyond to introduce new processes to book in Covid patients outwith hospital settings. The staff showed immense flexibility and changed their hours of work and their roles.The success of the CACs was due to the commitment, flexibility and team working across eHealth to support the Board in its response to the pandemic.

The speed of the Covid pandemic meant the NHS had to react quickly to the challenges.
The Medical Equipment Management team did just that. In March 2020 it was clear that we needed to increase our capacity to treat those who would inevitably become very ill with Covid.
The team used their technical expertise to convert 163 anaesthetic machines within days so they could be used as ICU ventilators. This was repeated for infusion pumps, ultrasound scanners, renal dialysis equipment, blood pressure monitors and thermometers. In total they configured 4200 pieces of equipment needed for Covid patients.
They also rolled up their sleeves to support the increased critical care pressure – volunteering to move from a five day a week operation to seven and volunteering willingly.

Queen Elizabeth Frailty Team has been running for six years and aims to improve outcomes for older adults and reduce the time they need to spend in hospital.
This has been successful and they managed to increase the proportion of patients discharged in less than 48 hours.
They also use imaginative ways to make a hospital stay more comfortable and the environment better for patients – through artwork, memory boards, ipads. They even created a 6m frailty therapy walk along the river Clyde- with places that patients would recognise around Glasgow.
Their relationships, their direction and the way they work and collaborate mean that they have been far bigger than working as individuals – and our patients have reaped the rewards of this.

The Frailty at the front door team was faced with a great challenge – to increase same day discharges for patients coming into the Queen Elizabeth with frailty issues. Patients are usually happier at home and recover better in their own environment.
The aim was to increase same day discharges from 15% to 25%.
During a week of rapid change – they worked with AHPs, pharmacy and mental health staff, nurses, ED Consultants and social work to ensure 12 hour a day cover, moving away from the 9-5.
The team worked together with a collective aim and shared values and managed to overcome a number of logistical challenges to ensure that care was delivered in a timeous, person-centred fashion.
The final outcome saw 30% of patients discharged within 24 hours.
This award commends staff who have implemented an initiative to improve the health and wellbeing of patients, the public and/or staff.
When Covid emerged in early 2020, the team at the West of Scotland Specialist Virology Service realised they would be at the forefront of testing for this new virus.
The team quickly set to work to ensure they had the right equipment to test for the virus and then developed a new test to detect it. At first they were carrying out tests for 75% of Health Boards.
Now, the lab is testing 1,500-2000 samples a day with a turnaround time of less than 24 hours. The team expanded their hours from 9-5 to 8-10 at short notice to meet demand and one person even came out of retirement to help.
The virology lab has been central to our pandemic response and has offered a very high quality service that clinicians – and patients – have relied heavily upon.

Tracy Brown is a Prescribing Support Pharmacist, based in the south side of Glasgow.
Recognising the needs of a large group of patients in the Govanhill area with chronic pain, she set up a Pharmacist Led Pain Clinic, accepting referrals from GP practices, using telephone appointments and online/ printed self-help material.
This was all done during the pandemic and while working from home, linking in with the Advanced Practice Physiotherapist, Links Worker and aYoga Pain Specialist.
The focus was on pain education and promotion of self-management of pain to help minimise prescribing of analgesics and to improve patient safety.
Outcomes from the project include reduced use of opioids, patients pain scores reducing by an average of 3 (on a 1-10 score) and a 36% reduction in GP appointments for pain issues from the previous six months.

As physiotherapists specialising in mental health, Angela and her team work regularly with service users who have a diagnosis of dementia. The main referral reason is due to falls and mobility issues.
There is a recognised exercise programme in existence, but the team recognised that many patients with dementia had difficulty following this, so they set about devising their own.
The worked with experts both within and outside the Board to get it right, looking at all aspects of the design including colours, colour contrast, layout, font size and type.
Feedback from the new programmes has been overwhelmingly positive – from across the UK. Word has spread – as far at the States, with families and professionals recognising this great example of patient-centred care.

Vaccination has been the buzzword of 2021 and NHSGGC’s rollout has been a massive undertaking.
The eHealth team was pivotal to this – working with the wider vaccination team to put together the technology, telephony, reporting and contact centre staffing required to support our programme. This included establishing a contact centre at very short notice.
It was also necessary to recruit staff, train them in the new system so they were able to deal with calls, book appointments and answer thousands of email enquiries.
The collaboration, flexibility and workload associated with this project cannot be understated and formed a key part of the Board’s response to the pandemic.
This award is for staff who have increased efficiencies taking a new approach to work making better use of resources.
One of the significant challenges of the pandemic was the lack of information about the virus, how it should be treated to best effect, and what it meant for our staff, their families and their patients.
The Communications and HR teams swiftly came together to formulate a process for rapid, real time employee communications and engagement to ensure that staff could retrieve the information they needed, when they needed it in the easiest possible way, but that there was also a mechanism by which staff could engage with decision makers in the Board so they could understand quickly what the ever changing roles they were undertaking required of them and likewise, where to go for help and support in the midst of a crisis.
With that, the all employee COVID dedicated email message service and COVID-19 web portal was created. The latter still remains in use and was utilised by Health Boards across Scotland as best practice and a useful guide for their staff. Feedback has been hugely positive and the resource has been massively well utilised throughout both NHSGGC and across Scotland.

This centre was set up in a particularly rapid timescale, collaboratively by eHealth teams who established a project approach to putting in place the necessary call centre accommodation, IT Kit, Telephony, data analysis and reporting. From initial recruitment to training to go live, eHealth teams worked together to rapidly establish the centre and Health Records co-ordinated all of the operational activity, training and support in the new roles to ensure patients were booked in a timely manner 24/7.

During the COVID-19 pandemic, waiting times for rheumatology patients to receive treatment from physiotherapists and occupational therapists were escalating as they couldn’t be seen face to face in a hospital setting.
While remote consultations were brought online, it became clear that patients needed to be seen face to face to assess more accurately and provide better, more successful treatment to improve their quality of life.
A one stop face to face clinic was set up at the NHS Louisa Jordan meaning that physios and OTs could assess the patient jointly and resolve several issues in one appointment.
This new approach rapidly reduced waiting times and 67% of patients said they were satisfied with the new model of care and the team received a lot of positive patient feedback such as how organised, friendly, happy, quick and efficient the process was, which was a great result for the team.
This award recognises the often unseen work of our staff who help make NHSGGC a better workplace, improving the culture and supporting colleagues.
In March 2020 thanks to the swift launch of Community Assessment Centres across NHSGGC, we were able to manage the flow of potential COVID-19 patients into our hospitals and GPs and minimise the risk of transmission. Barr Street was one of the first of such centres and the team there, made up of volunteers, had a huge impact on what would turn out to be an extremely important tool in the fight against COVID-19. The multi-disciplinary approach which saw teams working in a fast-paced, unknown and constantly evolving situation help reduce demand on hospital services and GPs and ensured those patients with COVID-19 symptoms were effectively managed without risk to others.

As resources shifted to meet new requirements during the height of the pandemic, so too did the demand for staff. At times the recruitment team were processing for 24 hours per day as they managed to employ staff for roles from estates, nursing, medical, test and protect and the vaccination rollout programme, among others. Whether onboarding, training or supporting the new workforce, there was no single team across the Human Resources Directorate which didn’t contribute to the effort and throughout the directorate has helped create new approaches and ideas which have modernised NHSGGC’s approach to recruitment, helping to maximise the pool of candidates available.

Over the past 20 months, there has been unprecedented change across our sites. There were no standard operating procedures for COVID-19. As such we’ve all had to change the way we work, but perhaps none more so than facilities teams who’ve been at the coal face throughout – supporting all other staff, ensuring the latest guidance on cleaning, PPE, pathways and protocols were being implemented. From the catering teams feeding staff and patients, to the porters, domestics, helpdesk and back office support staff – everyone in the facilities team at the QEUH has played a central role in ensuring we’ve been able to continue delivering person centred care throughout this pandemic.

With a huge increase in the demand for virtual services almost overnight, the eHealth team had the colossal task of ensuring acute and primary care services had the equipment and capabilities to deliver virtual consultations. This was crucial in allowing teams to look after patients while also keeping them safe from COVID-19. Since the beginning of the pandemic the system has been rolled out to thousands of services across acute and primary care, and is now used a regular means of delivering person care alongside telephone and face-to-face consultation. The role of the eHealth team in delivering this important service cannot be understated.
This award recognises staff who have travelled overseas to provide healthcare and/or education in developing countries or countries in crisis.
SAC Danny McInally is an RAF Regiment Gunner with 603 (City of Edinburgh) Squadron of the RAF Reserves.
This year Danny was mobilised and deployed to Romania on Operation BOLOXI. The detachment of four Typhoon fighter jets from 135 Expeditionary Air Wing (EAW) was based in south east Romania.
Deployed for five months, the EAW has been working alongside the Romanian Air Force to police the skies over the Black Sea. The RAF aircraft deployed to Romania were part of the UK’s contribution to reassurance measures, and to ensure the operational capability of NATO’s eastern flank. The Air Policing mission demonstrates NATO’s flexible capabilities and readiness, underlining the commitment of Allies to each other.
During the deployment Danny worked as part of a Flight (around 35 Gunners), ensuring that everything from the Typhoons flying, Engineers servicing the aircraft, to the Chefs feeding the detachment personnel, could operate without threat from possible adversaries.

Stuart Watson, Clinical Director for plastic surgery at GRI, has dedicated many hours of his personal time, both from home, and travelling to different countries in Africa, using his skills as a plastic surgeon, but also fund raising alongside this work.
At the start of COVID Stuart started running weekly one hour educational webinars from the Canniesburn Unit. For a year, these were hosted every week, and more recently every two weeks. This was initially designed to provide teaching for their own trainees, but the webinars became hugely popular and have consistently attracted international audiences averaging about 200 colleagues, from 30 to 40 different countries. There is a strong audience from Africa and the Middle East, including countries such as Yemen and Syria, where medical educational opportunities are scarce at present and outside contact is valued.
This award recognises nurse(s) who demonstrate the best qualities of patient care and the ethos of nursing.
The Tissue Viability Team (TVT) have set the highest standards of care, will managing the challenges of having part of the team redeployed to the ITU due to Covid. During a time where referrals increased the team created and implemented 42 service development initiatives to improve patient care. These initiatives included managing moisture, mattress safety guidance and product guidance for wards to help clinical staff choose form a selection of wound products and were designed to support clinical staff and ensure patient care was consistent and to the highest of standards. This approach led to successes such as a 100 per cent reduction in patients developing moisture damage and an 82 per cent reduction in the need for advanced wound care for radiotherapy. The development of a patient self-care information leaflet reduced pressures on district nurses and allowed them to prioritise their caseloads for those who could not self-care.

As the COVID-19 pandemic took hold, the Elective Orthopaedic Nursing Team adapted to turn an elective surgical ward into a COVID-19 ward, quickly learning new skills and knowledge which underpinned the delivery of excellent care to all patients. The team continually proved themselves to be invaluable to NHS Greater Glasgow and Clyde, tackling the enormous challenge of COVID-19, while bonding and carrying each other through the most difficult time of their nursing careers. The team have now refocused and switched back to their surgical nursing roles seamlessly, despite having no time to stop and recover from the impact of the previous 14 months.

In January 2020, it became clear to the infectious diseases inpatient service for GGC at ward 5C of QEUH, that they would need to be prepared to manage potentially significant numbers of patients with Covid-19. The infectious diseases nursing staff, put patient’s health before their own before it was clear just what the impact of Covid-19 would be, while helping to inform the patient pathways and clinical care for the first Covid-19 patients, while emotionally supporting isolated patients and their families.
Throughout the pandemic, this team have continued to adapt, while demonstrating the highest standards of nursing.

The team at the Gorbals Health Centre Treatment Room, particularly Gayle, provided an exceptional treatment plan for a patient, who believed she was facing a possible amputation because of damage to her legs. This transformed her quality of life in just 12 weeks, following four years of frustration and trying to manage pain.
Gayle instilled hope in the patient that she could still make a full recovery and stayed with her on every step of her journey, showing compassion, dedication, with her abilities reducing anxiety. Gayle was supported by an excellent reception staff team, an efficient appointments system and a friendly although professional approach.
The patient said Gayle has given her “a new lease of life”, which has seen her successfully apply for a new job.
Recognising people who go the extra mile contributing tirelessly and providing outstanding help and support for the benefit of others.
At the height of the COVID-19 restrictions, the RAH Volunteer COVID Response Team played a crucial role in delivering essential items to inpatients, with visiting restricted.
The Befrienders service has supported patients and their loved ones throughout the pandemic, with volunteers being continually praised for their reassuring and caring nature, hard work and professional manner, at a time when the community needed them most.
Volunteers worked tirelessly to deliver parcels of personal items to wards, helping to keep lines of communications open between families, loved ones and those isolated in hospital and providing comfort.

Staff R&R Hubs were set up at the start of the pandemic to support staff and help them unwind from the pressures they were facing as frontline workers. Volunteers organised by the Volunteering Service, including 100 volunteer airline staff from ‘Project Wingman’, joined staff in operating the Hubs, providing a friendly ear and cup of tea whenever needed.
The volunteers provided 24/7 cover during the toughest months of the pandemic, the Project Wingman staff attended in airline uniforms with the aim of providing an airline first class lounge service to our staff. They were responsible for completely transforming the atmosphere and physical spaces in the R&R Hubs into places where people really wanted to visit to unwind.

Chiara Galimberti came forward as one of the first Covid Pandemic Response Volunteers to offer support to NHSGGC in March 2020. Chiara, who is from the North of Italy had watched the catastrophic impact of the pandemic there and wanted to help as a thank you to the people of Scotland for their hospitality.
Chiara has become a key member of the RAH Pandemic Support Volunteer team supporting staff and our patients with tasks such as managing hand sanitising stations, supporting staff in PPE donning, running staff hubs and the large scale volunteer led Give & Go service. Chiara did all this while not being able to see her family for 18 months.
Passionate about making a difference and helping others, Chiara has faced every challenge with positivity and compassion.
The NHSGGC staff Excellence Awards are looking for patients, visitors and staff to nominate our dedicated teams and individuals. Our staff truly have gone above and beyond in this past year and a half and we want you to tell us about your experience of outstanding care.
These prestigious awards are for individual members of staff, teams, or projects that have identified ways to deliver improvements that benefit patients and service uses, colleagues, or NHSGGC.
Staff, patients and visitors can all nominate in these awards. We want you to tell us about the dedicated teams and individuals who go to extraordinary lengths to provide exceptional care for people who use our health services.
But we’re not just looking to celebrate the tremendous efforts of our staff. We are also looking for services that staff have moulded to patients’ needs, or projects that have transformed the way we work.
There are seven categories in our Excellence Awards, so there is a category to fit every project, programme, or an outstanding member of staff.
They are:
Our awards are a brilliant opportunity to shine a light on someone you know, who goes above and beyond the call of duty, to provide exceptional care and support.
We know our staff provide incredible patient care but we need you to tell us your stories.
The closing date was Wednesday 19 February 2025.