Please see the consensus statement on metastatic surveillance of uveal melanoma in Scotland. This gives up to date information on how often we check your body for spread of eye melanoma.
Services A to Z
Service Overview
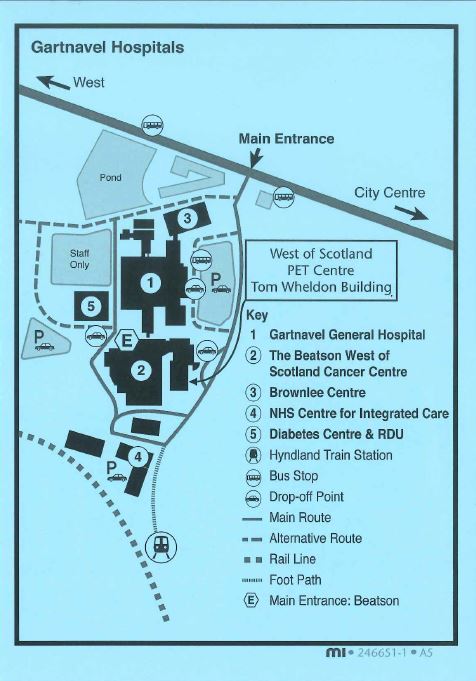
The Molecular Radiotherapy (MRT) service offers a range of radionuclide therapies at Gartnavel General Hospital (GGH) and The Beatson West of Scotland Cancer Centre (BWoSCC) and is staffed by a friendly and professional multi-disciplinary team. The team includes medical doctors, technicians, nurses, physicists, healthcare support workers and clerical staff. Therapies take place in either Beatson main out patients, ward B3 or Nuclear medicine GGH.
Opening Times
Monday to Friday, 8.30am – 4.00pm (Closed Public Holidays & weekends)
Change / Cancel Appointment
If for any reason you are unable to attend your appointment, please inform us by telephoning 0141 301 7621 as soon as possible during office hours to contact your nurse specialist. We will make every effort to adjust your appointment.
Location
Therapies take place across multiple sites on the Gartnavel campus. Please see your patient info leaflet, which will come with your appointment, for location details.
Contact Details
- Main nuclear medicine department number – 0141 301 7900
- Ward B3 number – 0141 301 7623
- Clinical Nurse Specialist – 0141 301 7621
Additional Information
Was this helpful?
Service Overview
The Beatson West of Scotland PET centre is located on the Gartnavel Hospital Campus. If you have been referred for a PET-CT scan, we will post you an appointment letter, patient information leaflet and directions to the PET Centre. These should provide all the necessary information regarding where and when to attend, what preparation is required and answer many other questions you may have. However, should you have any further queries regarding your PET-CT scan, please call the department on 0141 301 7800 and staff will be happy to help.
Below is a video of what to expect when attending the department for a PET scan. Subtitles can be enabled in the settings menu at the bottom right of the video.
Additional Information
- FDG PET CT Scan – patient information leaflet
- PSMA PET CT Scan – patient information leaflet
- Contrast Enhanced FDG PET CT Scan – patient information leaflet
- Ga-68 Dotatoc PET CT Scan – patient information leaflet
Location
The West of Scotland PET Centre is on the Gartnavel Hospital Campus in the Tom Wheldon building of the Beatson Cancer Centre;
1053 Great Western Road, Glasgow, G12 0YN
Scottish Ambulance Service
The Scottish Ambulance Service has a central booking service which allows you to book ambulance transport. If you require this service, please phone 0300 123 1236 at least 3 days before your appointment but no sooner than 30 days in advance. Lines are open from 8.00am to 8.00pm Monday to Saturday.
Voluntary Hospital Transport Service
There are several options available if you require Hospital Transport Services to attend your appointment. Please see contacts below:
- East Dumbarton Voluntary Drivers – 0141 280 9527
- Lanarkshire Voluntary Drivers – 01698 355 137
- Ayrshire Voluntary Drivers – 0156 353 8008
Department Contact Details
- Call: 0141 301 7800
Other Useful Links
- Nuclear Medicine at Gartnavel General Hospital
- PET-CT national referral criteria
- PET-CT referral form & guidance
Was this helpful?
The Orthopaedic Research Department is situated in the Department of Orthopaedic Surgery at the Glasgow Royal Infirmary. We conduct a variety of clinical and basic research as well as exploring service redesign to improve the patient pathway through clinic.
Our clinical research portfolio revolves around the use of new robotic guided knee replacement surgeries to improve surgical accuracy, patient recovery and improve patient gait following knee replacement. We also assist in the recruitment of patients to trials that are centred outwith the Glasgow Royal Infirmary. Examples of these clinical trials can be found clicking the research link below.
As an active research department we frequently disseminate our research findings in journal articles. A list of these publications can be found via the publications link below.
If you would like more information on the research activities currently on-going in the Department or to discuss participating in an on-going clinical trial please contact: iii-ortho-research@glasgow.ac.uk
Permission to access patient records
We are seeking approval for permission to review the medical records of patients that took part in our two previous clinical trials, TRUCK and MAKO. This would involve seeking ethical approval to access patients’ medical records to record details of health care usage which is both related and un-related to their knee replacement. This is performed in an anonymised manner and only extracts information about how many times a participant has accessed a health care provider, with no details as to the reason for their visit. The aim of this new aspect of the study is to to review the participants retrospective NHS healthcare usage in a non-identifiable way to see if there is any downstream, long term differences between the patients who were randomised to receive the robotic-assisted knee surgery and conventional knee surgery groups. The difference in health care usage may highlight a potential cost benefit of the use of robotic or conventional surgery.
For access to the NHS Greater Glasgow and Clyde Data Privacy Notice, please follow the link below. This includes a section on data protection in Research and Innovation.
News
Information on upcoming projects and future collaborations, coming soon.
Upcoming Trials
Charity
Hip & Knee School
Was this helpful?
Within the team there are many years of experience in orthopaedic nursing and the nursing staff have many specialist skills in caring for orthopaedic patients. In our department you will meet nurses trained in caring for you from your first visit, to pre-operative assessment and follow up.
Mairi MacKinnon – Limb Reconstruction Clinical Nurse Specialist

Mairi MacKinnon is the Limb Reconstruction Clinical Nurse Specialist based at Glasgow Royal Infirmary. She has recently joined the limb reconstruction team having previously served within the orthopaedic department as the musculoskeletal oncology nurse specialist for over 2 years.
Mairi manages all limb reconstruction patients including patients with external fixators, in particular, circular frames. She also assists the Intramedullary Nail Clinic where all tibial patients attend for review. As part of her role within the limb reconstruction service, she manages complex surgical wounds and has extensive experience in Negative Pressure Wound Therapy.
Pamela McKirdy – Orthopaedic Staff Nurse

Pamela McKirdy is a Staff Nurse in the Orthopaedic Outpatients Department. She has worked in Orthopaedic Outpatients for 24 years gaining a wealth of experience and knowledge in Orthopaedic conditions, trauma and elective surgeries and wound care. She has completed the casting course and has specialist training and experience in managing both elective and trauma surgeries post-operatively and on many occasions it may be Pamela who will review your condition or surgery in a stand-alone clinic where your entire care will be managed by experienced nurses and your x-rays reviewed. She is able to consult directly with senior medical staff if appropriate regarding any unusual findings.
Sarah Vaughan – Oncology Clinical Nurse Specialist
Sarah is the Clinical Nurse Specialist for the Musculoskeletal Sarcoma Oncology Service based at Glasgow Royal Infirmary. Sarah recently joined the team having previously worked as an Oncology Clinical Nurse Specialist for 6 years within another Trust.
The Oncology team form part of a specialist service who have extensive knowledge and expertise in managing Sarcoma. This team provides a comprehensive service that covers investigation of suspected disease, diagnosis, treatment and follow-up.
It’s Sarah’s job to provide support throughout this time, offering advice and a point of contact whilst patients undergo investigations and/or treatment.
Was this helpful?
The Extended Scope Physiotherapy Practitioners (ESP) are specialist clinicians who have undertaken additional Orthopaedic training. They work in a similar role to the Consultants within the Orthopaedic Outpatient Clinics at Glasgow Royal Infirmary.
During your clinic appointment, the ESP will carry out an assessment of your problem and if necessary, organise further investigations (e.g. X-Ray, MRI).
Please wear suitable clothing to allow assessment of the relevant joint.
Some investigations such as MRI scans cannot be carried out in clinic and a further appointment for this will be organised. Results of the assessment and/or any investigations will be reviewed by the ESP who will discuss the available treatment options with each individual patient.
If further intervention by surgery is indicated, this will be discussed during the clinic appointment. If other management options are more appropriate e.g. onward referral to other services, this can also be organised.
Useful Internal Links
External Links
ACL Reconstruction Rehabilitation
Frank Gilroy’s ACL reconstruction rehabilitation programme (opens on a new page)
*NOTE: your physiotherapist will provide you with a password in order to access this programme.
Joint School App
Sign up and download necessary https://www.jointschool.app (opens on a new page)
The Royal College of Anaesthetists
leaflets and videos on the types of anaesthetic that may be used for your surgery www.rcoa.ac.uk (opens on a new page)
Was this helpful?
- Trauma and Orthopaedic Consultant Surgeons
- Trauma and Orthopaedic Extended Scope Physiotherapist Practitioners
- Trauma and Orthopaedic Advanced Podiatry Practitioners (APP)
- Trauma and Orthopaedic Specialist Nurses / Nursing Team
- Trauma and Orthopaedic Trauma Coordinators (Coming Soon)
- Trauma and Orthopaedic Musculoskeletal Oncology Service (Coming Soon)
Was this helpful?
Anaesthesia allows you to be pain free and comfortable during your operation. Sometimes this involves a general anaesthetic which is a state of controlled unconsciousness controlled by medication during which you will not feel pain or remember anything. This is often referred to as ‘going to sleep’ for your operation. However, anaesthesia does not always mean that you have to be unconscious as modern anaesthetic techniques can numb certain parts of your body such that you will not feel any pain whilst still being able to remain awake. These techniques can numb a small part of your body (local anaesthesia), an entire arm or foot (nerve block) or the lower part of your body from the waist down (spinal or epidural anaesthesia). There are lots of benefits to having a procedure done in this way and for some orthopaedic operations, such as hip and knee replacements, these have become the most common types of anaesthetic. They can often be accompanied by sedation if required for your comfort. Sometimes however these techniques are not the best option for you and a general anaesthetic will suit you better or indeed the operation cannot be done without you having a general anaesthetic.
You will hear more about the anaesthetic options for your intended operation when you attend your pre-operative assessment. Please ensure you pick up a copy of any relevant information leaflets and take time to read through them. You may also be given the opportunity to watch a video prior to your operation if you are having a knee or hip replacement.
Your preferences are important and you will be given the opportunity to discuss the risks and benefits of the anaesthetic options available to you. In some instances you may be asked to attend the hospital specifically to see an Anaesthetist if the specialist nursing staff in the pre-operative assessment clinic feel this would be of benefit to you, but in most cases you will meet your Anaesthetist on the day of surgery.
Details about what to expect and the potential side effects and complications of the different Anaesthetic options are outlined in the document link below ‘Anaesthesia: What you need to know’. Please take the time to read it so you are better prepared for the day of your surgery.
Anaesthesia Information leaflet
Your Anaesthesia for Orthopaedic Surgery
Was this helpful?
You can find information on how to get to both Glasgow Royal Infirmary and Stobhill ACH and both site maps by clicking on the appropriate box below.
Patient Transport
If you are unable to make your own way to your hospital visit due to a medical condition or mobility issue and require ambulance transport to get to your healthcare appointment then please click on the link below which will take you to our Patient Hospital Transport page which gives you all the relevant information on how to arrange this.
Was this helpful?
If you have been advised by the medical team caring for you that you may benefit from having a hip or knee replacement then the following information and associated links will help ensure you are as prepared as you can be for your surgery and recovery.
Most total hip and knee replacements take place at Glasgow Royal Infirmary. If you are having a Uni-compartmental knee replacement (‘Half-knee’) then you may be advised that you can have your operation carried out at Stobhill hospital if the surgeon feels this would be appropriate for you. If this applies to you then please follow the Stobhill Hospital information where relevant.
[ Given the current unprecedented pressures on our NHS and orthopaedic services at Glasgow Royal Infirmary, we would like to offer you the possibility of remote support via the NHS Joint School App for detailed information on your condition, planned procedure and ways of managing your symptoms whilst awaiting your surgery.]
Your Joint Replacement Pathway
Pre-Op Assessment
You will be invited to attend the pre-operative assessment clinic before your operation. You will meet one of the specialist nurses who will ask you questions about your health and arrange appropriate tests such as blood tests and an ECG (heart tracing).
If any issues are identified that may require further investigation or advice the pre-assessment nurses will then speak to an Anaesthetist. You will be advised of any changes or further tests following this and may be asked to come back for a second appointment to meet an Anaesthetist in clinic. This is generally to explore your health further and discuss the anaesthetic options or risks in more detail. Occasionally an issue is identified that warrants further investigation or treatment before you proceed to surgery. If this is the case the nursing staff will explain what is required and how to let them know when this has been done and you are ready to move forward to surgery.
This process is designed to make sure you are as physically ready for surgery as possible and also gives you information about what to expect so you can take time to think about whether you still want to go ahead.
Please bring your medication with you to the pre-operative assessment clinic or a complete list of these with your prescription. Most medications should be taken as normal up to and including on the morning of surgery. There are a few specific medications that may need to be stopped prior to surgery or not taken on the morning of surgery. These are usually ‘blood thinning’ medications such as clopidogrel, warfarin, and aspirin. Your pre-operative assessment nurse will give you specific instructions.
Download our specific Covid related Pre-Op Self-Isolation Advice leaflet here
Preparing for Your Surgery
If you can improve your general fitness, strength and well-being prior to surgery you will find that your recovery is easier and quicker. It may also reduce the risk of complications. A hip or knee replacement is a major surgical procedure that places physical demands on your body during the surgery and anaesthetic and during the healing process. It also requires effort on your part to recover well and get maximum benefit from your new joint such as performing regular physiotherapy-guided exercises.
Watch the video to see what you can do to prepare for surgery.
Click here for more videos on how to improve your fitness before and after surgery.
If you are Overweight
Reducing your weight will reduce many of the risks of having an anaesthetic. Importantly, it will also reduce the load carried by your hip or knee and can reduce the pain in the joint even prior to surgery. It will make your recovery and physiotherapy easier after surgery too. There are multiple sources of information and local groups to help you learn about healthy eating and lose weight.
The NHS inform website can provide a useful starting point – Food and Nutrition . Your local GP surgery may be able to point you in the direction of nearby groups or services if you wish.
If you Smoke
Giving up smoking as far in advance of the surgery as possible will reduce the risk of breathing problems both during and after your anaesthetic and reduce the risk of problems such as a chest infections. If you need help or advice with this from a trained advisor please contact Quit Your Way on 0800 84 84 84. Lines are open Monday to Friday 8.00am until 10.00pm and Saturday to Sunday 9.00am until 5.00pm. You can also visit the Quit Your Way website to find a local Quit Your Way Pharmacy Service.
Eating and Drinking the day before surgery
Please follow the advice below.
Note: ‘Clear fluids’ includes water, black tea or black coffee (no milk).
If you are asked to come to the hospital for morning surgery
Eat your evening meal as normal on the day before surgery
Have a snack in the evening if you want
Do not eat anything after midnight
Drink only clear fluids after midnight
Drink clear fluids when you are thirsty until 0600
Have a drink of around 300ml of clear fluid at 0600 to help stop you getting thirsty and improve your comfort while you wait.
If you are asked to come to the hospital for afternoon surgery
Have a light breakfast before 0700 on the day of surgery to keep you feeling comfortable during the day ahead
Do not eat anything after 0700
Drink clear fluids when you are thirsty until 1100
Have a drink of around 300ml of clear fluid at 1100 to help stop you getting thirsty and improve your comfort while you wait.
The exact time of your surgery may not be confirmed until on the day as you will be part of a theatre list with other patients. We ask more than one patient to arrive for the start of the day to help ensure flexibility if there are last minute changes and to allow the theatre staff to see you before the surgical session begins. If there will be time for you to have a further drink of clear fluid on arrival at hospital the nursing team will be able to advise you of this on the day.
Your Anaesthetic for Joint Replacement Surgery
Anaesthesia allows you to be pain free and comfortable during your operation. In some cases, especially knee replacement surgery, your anaesthetist may place a longer lasting local anaesthetic around other nerves in your leg to help reduce the discomfort for a little longer after surgery. This is known as a “nerve block”. They will discuss this with you on the day of your operation.
There are occasions where, for medical or surgical reasons, a spinal anaesthetic is not suitable and your anaesthetist will be able to discuss the options with you. This often includes a general anaesthetic. Your preferences as to the type of anaesthetic you receive are also important so please take the time to consider these and ask your anaesthetist for advice. In some instances you may be asked to attend the hospital specifically to see an anaesthetist if the specialist nursing staff in the pre-operative assessment clinic feel this would be of benefit to you. In most cases you will meet your anaesthetist on the day of surgery.
You can download this patient information leaflet – Anaesthesia: What you need to know and watch this short video by your anaesthetist.
For further information https://www.nhsggc.org.uk/your-health/health-services/orthopaedics/anaesthesia/
Enhanced Recovery After Surgery [ERAS]
The ‘Enhanced Recovery After Surgery Programme’ simply refers to the processes that are in place to ensure you are prepared for your surgery and receive the care required to get you back to the comfort of your own home as quickly as possible.
Evidence tells us that a huge part of improving a patient’s recovery after surgery is making sure they have a good understanding of what to expect before coming into hospital. This website together with information leaflets and appointments with the staff in the hospital are all opportunities to find out about what will happen when you come into hospital and how to prepare.
The operation itself and healing process place high physical demands on your body. In the weeks and months before your operation you can take actions to improve your health and fitness in preparation for surgery. If you do this then you will be back to your normal self much more quickly and hopefully gaining the benefits of your new hip or knee as soon as possible.
We also aim to make sure all patients get the same high level of care during their anaesthetic and surgery and afterwards on the ward so we can get you back on your feet as soon as possible. Getting out of bed with the help of the physiotherapists and nursing staff soon after surgery, eating and drinking normally, getting dressed into your own clothes and getting home as soon as possible have all been shown to get your recovery off to the best possible start and do not increase the risk of any complications.
Evidence tells us that the sooner you can get your new hip or knee moving and back on your feet the better the result from your surgery. It also helps reduce the discomfort in your new joint. We will ensure you have plenty of medication available to help ease the pain when you need it. In most cases the discomfort significantly improves after only a few days.
You will be told how long your hospital stay is likely to be when you come into hospital so you know what to expect. The planned duration of stay will vary depending on the specifics of your operation and which hospital you are attending. You will be assessed regularly after your surgery to check how you are progressing and to monitor for any complications. You will be discharged home when you are ready even if this is earlier than the planned date. If you need a little more help don’t worry, you will not be discharged until you are ready.
Click here (https://www.nhsggc.org.uk/your-health/health-services/orthopaedics/hipknee-replacements/exercise/) for some videos on how to improve your fitness before and after surgery
