These guidance notes refer to different parts of the ACP Summary on Clinical Portal.
“Anticipatory Care Planning” becoming “Future Care Planning”
In relation to the recent letter from the CMO regarding the name change from “Anticipatory Care Planning” to “Future Care Planning” on 20th September 2023, we wanted to remind all staff of the current process by which people can share their views and wishes when it comes to future care and treatment within NHSGGC. We also wish to highlight the resources available to support both staff and the public.
Since 2019 we have been storing information about future care planning on the “Anticipatory Care Plan Summary” which sits on Clinical Portal. This document can be edited by any member of staff to record people’s wishes and preferences. It also gives the opportunity to document clinical management plans, record Power of Attorney details as well as DNACPR discussions. A copy of this document is automatically shared with GPs who can update information on the Key Information Summary (KIS). Primary Care staff can read the latest ECS and KIS directions from Scottish Government here. Staff should check both KIS and the ACP Summary to ensure they have all information available.
Within the Board, we believe future care planning is everyone’s responsibility. This is one of the reasons that we have chosen the Clinical Portal system to store future care planning information as it is accessible by Acute, Community and Primary Care as well as Social Work. This means that the majority of health and social care professionals can access and update this information.
We acknowledge that different services will have different conversations based on the roles and remits of the team, however by bringing this information into a central location we can easily share information and help to create person-centred care plans which reflect the wants and needs of people. Therefore our ACP Summary should not be viewed as the responsibility of one individual or service, but rather a dynamic document with many people contributing information.
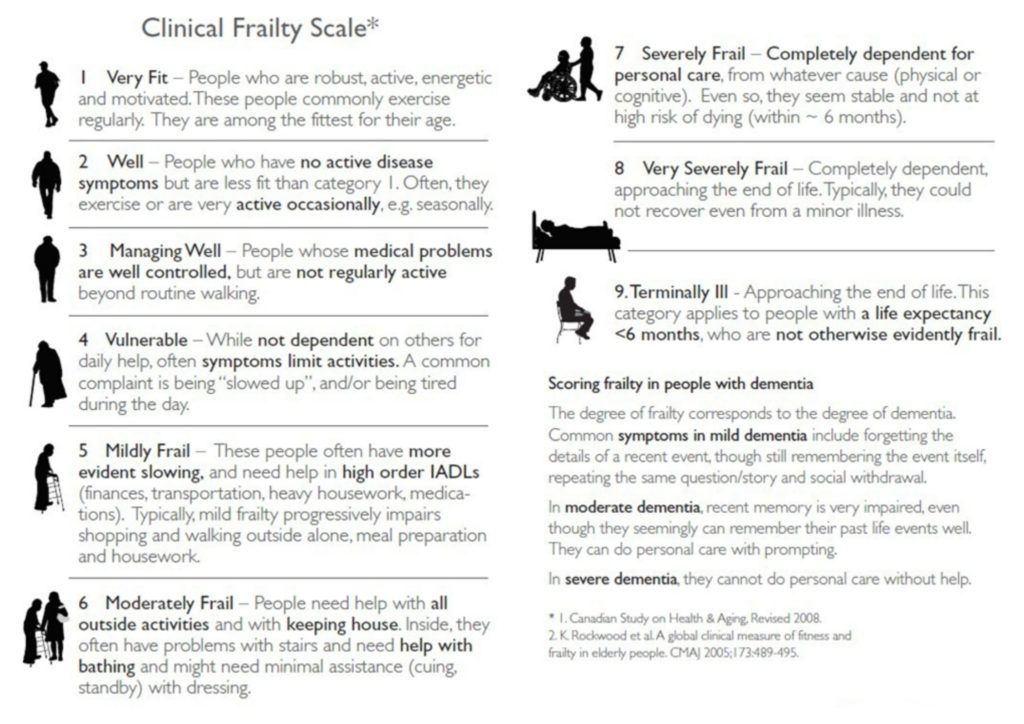
It is also worth re-iterating that conversations about future care should not just be limited to people at or nearing the end of their life. These conversations can be useful for people at any age and stage of their life and the level of planning required will depend on where someone is in their life journey. We are also encouraging all staff to consider whether someone could benefit from a Frailty Assessment using the Rockwood Clinical Frailty Scale, the results of which can be recorded on the online summary. Early identification and monitoring of frailty is important to help create plans which can slow decline or in some cases reverse frailty. From more information about the Clinical Frailty Scale staff can attend an overview session – more details available on the Training Hub.
The Anticipatory Care Programme, which launched in April 2020, is available to support all staff across the Board with information and training. There is an eModule and a variety of virtual training delivered by the ACP Team and Realistic Medicine Teams including walkthroughs of Clinical Portal and communication skills with case studies to discuss. All training is open to all staff in any role and at any level. For more details please visit the Training Hub.
The ACP Team have also created a wealth of resources for the public including webpages which explain many different aspects of future care planning. They have leaflets which can be printed off with further information (these can be found on the Useful Documents and Resources section of the webpages) and also regularly host events covering various topics – these are open to both staff and the public.
Over the coming months we will be working closely with members of the Scottish Government to ensure that the work that has already taken place in GGC can be shared with other Health Boards and that we continue to align with any national programmes and messaging. We will also continue to work with colleagues in various services and programmes including the Realistic Medicine Team and Unscheduled Care.
We will also begin to change some of the language we use, particularly in public facing areas, to reflect the new term “Future Care Planning”, however during this transition period the phrase “anticipatory care planning” and “ACP” may still be used. The form on Clinical Portal will continue to be called the “Anticipatory Care Plan Summary” until further notice.
Full details of the approach to Anticipatory Care Planning/Future Care Planning within NHSGGC can be found in the Guidance/Standard Operating Procedure Document. Please note this will be updated to reflect the new terminology in coming months.
You can contact the ACP Team at ggc.HomeFirst@nhs.scot with any questions or for further information.
Consent
We do not require explicit consent to share the information contained within the Future Care Plan. Therefore the Future Care Plan Summary no longer records if someone has given consent to have a Future Care Plan.
A Future Care Plan is a document brings many pieces of information together into a shareable format. Therefore by engaging in a Future Care Plan conversation, the individual (or legal guardian) is agreeing to share this information.
Article 6(1)(e) of the UKGDPR in conjunction with the Intra NHS Scotland Sharing Accord allow the information contained within this document to be shared with Primary Care and other NHS Boards including NHS 24 and Scottish Ambulance, without the need for explicit consent. We are sharing this information for routine patient care as part of our Board’s duty to provide healthcare to our patients. It is best practice for staff to make sure the individual and/or their legal proxy is aware this information will be shared when conducting ACP conversations. If the patient would like further information about how the Board uses their data it can be found in our Privacy Notice here – https://www.nhsggc.org.uk/patients-and-visitors/faqs/data-protection-privacy/#
Recording whether someone would like to share information via Future Care Planning
Although we no longer record consent on the Future Care Plan Summary, the summary does include a question about whether or not an individual (or their legal guardian) wishes to have an Future Care Plan.
By asking this question we hope to enable staff to evidence when a conversation takes place, but the offer of a Future Care Plan is declined. We will monitor this data.
If a Future Care Plan is refused, staff have the opportunity to record the reason for this. We would ask all staff to complete this in order to provide context to their colleagues who may wish to revisit the conversation at a later date.
Clinical Frailty Score (Rockwood)
We would encourage all staff to consider carrying out a Rockwood Frailty Assessment and select the appropriate score in the Future Care Plan Summary.
If a frailty assessment is not applicable please select “0 – Not Applicable”.
Frailty Score Guidance (you can also download an app – Clinical Frailty Scale (CFS) – to help with the assessment – download for apple or android).
Special Notes / What is important to the individual?
Overview of person including family circumstances, accommodation information, health goals, what matters to them, emergency planning information etc. If person is a carer, or has informal carers please state too.
If person lacks capacity ensure this is recorded alongside who has been present during any discussions.
If a person declines a Future Care Plan, staff are encouraged to ask permission to record this decision on the Future Care Plan Summary so that other services are aware that a Future Care Plan has been offered. It is also best practice to indicate whether the person may be willing to revisit these conversations at a later date. Please record this in the appropriate question.
Current Health Problems / Significant Diagnoses
Overview of health issues and diagnoses. Baseline functional and clinical status to help clinician identify deterioration – e.g. baseline O2%, 6-CIT score, level of mobility, current or planned treatments.
It is good practice to indicate if there are any treatments or interventions that the person would not wish. If they have an Advanced Directive this can be indicated.
My preferred place of care
Depending on the person’s own circumstance and health journey, this may include preference about:
- long term care (e.g. nursing or residential care)
- place of treatment. This could include short or long term treatment.
- place of death
This section may also include the current level of care being provided by informal carers and/or any discussions which have occurred regarding on going and future care they may be able to provide.
My views about hospital admission / views about treatments and interventions / family agreement
It is best practice to give as much information as possible regarding views about hospital admission and explore with people what might happen in different scenarios. For example people may be willing to be admitted for a short period for symptom management, however would be unwilling to be admitted if it was likely they would be in hospital for long periods.
For people who are frail, in residential/nursing homes or approaching the end of their lives, it may be useful to discuss the 3 following scenarios:
- If you had a sudden illness (such as a stroke or a heart condition), how do you think you would like
to be cared for? - If you had a serious infection that was not improving with treatments we can give in the community like antibiotic tablets or syrup, how do you think you would like to be cared for?
- If you were not eating or drinking because you were now very unwell, how do you think you would like to be cared for?
