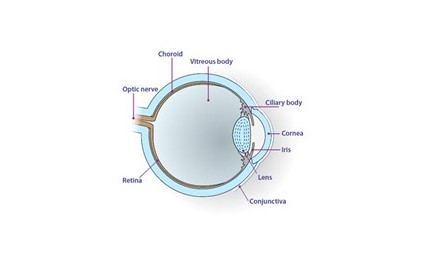
This sections looks at the different types of tumours that affect the conjunctiva (“the skin” of the eye, which helps protect us from infections).
Please see the conjunctival tumours below.
Ocular Surface Squamous Neoplasia
a) What s ocular surface squamous neoplasia?
Ocular surface squamous neoplasia is pre-cancerous or cancerous changes to the surface of the conjunctiva. Pre-cancerous changes can cause a condition called conjunctival intraepithelial neoplasia. This condition can turn into squamous cell carcinoma, which is a sinister tumour. This can spread onto the cornea causing decrease in vision. It usually affects one eye and is caused by sun damage.
b) What are the symptoms of ocular surface squamous neoplasia?
A fleshy pale lump is usually noticed on the surface of the eye next to the cornea. It may grow onto the cornea and, if large, can cause:
• Grittiness to the eye
• Watering
• Blurring of vision
Sometimes it can grow form the conjunctiva onto the eye lid.
c) What are the risks of getting ocular surface squamous neoplasia?
Risk factors for this condition include:
• Sun damage
• Fair skin
• Older age
• Conditions decreasing the immune system (e.g. HIV)
d) Will I need any tests?
In the clinic we may take pictures of the front of the eye. It is difficult to tell apart conjunctival intraepithelial neoplasia (pre-cancerous) from squamous cell carcinoma (cancerous). If the abnormal area is removed with surgery then it is sent to the laboratory to help confirm the diagnosis.
e) What is the treatment for ocular surface squamous neoplasia?
The main treatment is surgery (surgical excision). We may, however, use freezing treatment (cryotherapy) and Mitomycin C (MMC) eye drops as well. MMC can, however, irritate the eye. To treat this we may provide you with lubricant or steroid eye drops.
Primary Acquired Melanosis
a) What is primary acquired melanosis?
Primary Acquired melanosis (PAM) is newly formed brown pigmentation of the conjunctiva. People with white skin are more likely to get this. It usually affects one eye only. There are two different types of PAM: ‘PAM without atypia’ and ‘PAM with atypia.’ PAM without atypia is benign with no risk of transformation into melanoma. PAM with atypia, however, can turn into melanoma. Around 3 out of 4 conjunctival melanomas come from PAM with atypia. If you have dark skin, brown pigmentation of the conjunctiva from birth is very common and usually affects both eyes. This is known as conjunctival epithelial melanosis and is not likely to progress to melanoma.
b) What are the symptoms of primary acquired melanosis?
Uneven, painless, newly formed brown pigmentation is usually noted on the white of the eye. If the pigment is growing quickly or changing colour then it is more likely to be a conjunctival melanoma.
c) Am I likely to get primary acquired melanosis?
If you are middle aged and fair-skinned you are more likely to get primary acquired melanosis.
d) Will I need any tests to exclude melanoma?
If it is felt to be PAM without atypia we may take pictures in the clinic to help us monitor change. Sometimes a biopsy of the pigmented area, however, is needed to exclude cancer. When doing so we try to remove all of the pigmented area. The following features make us more likely to biopsy:
• Larger than 5mm
• Increasing in size
• Has thickened the conjunctiva
• Has a distinct nodule arising within it (pigmented or non-pigmented raised area)
• Has feeder vessels (blood vessels running into the pigmented area)
• Involving the cornea
• Involving the conjunctiva under the eyelids
• Previous melanoma
e) Is treatment needed for primary acquired melanosis?
PAM without atypia can be monitored in the clinic. The main treatment for PAM with atypia is surgery (surgical excision) with or without freezing therapy (cryotherapy) and Mitomycin C (MMC).
Conjunctival Melanoma
a) What is conjunctival melanoma?
Melanomas are tumours which come from pigmented cells in our body. As well as growing on the skin, they can grow on the conjunctiva of the eye. Conjunctival melanoma accounts for 2% of eye cancers. It arises most commonly form primary acquired melanosis, or from a naevus (freckle) already present on the eye. Least commonly it arises on its own; this is known as primary conjunctival melanoma. This cancer can spread to other organs in the body, most commonly, the liver.
b) What does conjunctival melanoma look like?
Conjunctival melanoma looks like an uneven, raised, grey or pink lump growing on white conjunctiva or from a pigmented area on the conjunctiva. This may cause irritation and watering from the eye.
c) What are the risks of getting conjunctival melanoma?
The following increase your risk of developing conjunctival melanoma:
• Having pale skin
• Red or blond hair
• Blue eyes
• Over 50 years of age
• Large number of moles or freckles
• Poor immune system (e.g. HIV)
d) How likely is the conjunctival melanoma to spread around the body?
There are some features that increase the risk of the melanoma spreading. These include:
• Large tumours (large basal diameter, and tumour thickness of greater > 2mm)
• Nodular tumours (rounded and raised)
• Tumour involving the eyelids
• Tumour involving the corner of the eye near the nose (plica or caruncle)
If the tumour has grown on white conjunctiva instead of a pigmented conjunctiva, then the tumour may be more aggressive. Most common place is the liver. A liver ultrasound scan is arranged at your local hospital every year to exclude spread of disease.
e) Will I need any tests?
A biopsy may be required to confirm the diagnosis. If we decide to biopsy we usually remove the whole abnormal area. We may perform CT or MRI scan to make sure the melanoma has not spread to other parts of the body. If the tumour is greater than 2mm thick or growing in the corner of the eye we may need to consider doing a sentinel lymph node biopsy (SLNB). This is where a sample is taken from the glands that drain fluid away from the eye and analysed for tumour cells. These glands are found at the front of the ear and in the neck. This is the first place the tumour spreads to before metastasising around the body. This procedure is carried out in the Queen Elizabeth University Hospital in Glasgow with help from our maxilo-facial surgeon colleagues. If the SNLB detects cancer cells then the glands can be removed with surgery or treated with radiotherapy.
f) What is the treatment of conjunctival melanoma?
Surgery (surgical excision) is performed with or without:
• Cryotherapy
• Mitomycin C (MMC)
• Radiotherapy
• Chemotherapy
Sometimes the tumour is too big or has spread behind the eye. In these situations enucleation may be the best option. If there is involvement of the eyelids or of tissue behind the eye, we may have to consider exenteration. If there is spread of disease to the lymph nodes in the neck, we may have to remove these or treat with radiotherapy.
g) Can the conjunctival melanoma come back after treatment?
Unfortunately the answer to this is yes. Even if the tumour is completely removed there is always a chance of the tumour re-growing in the same place or in other parts of the body. For this reason, we monitor in the clinic after treatment.
Lymphoma
a) What is lymphoma?
Lymphoma is a condition where the white cells that usually fight infection are “out of control”, keep dividing, and do not die. These abnormal cells can collect and grow in the lymph nodes. They can, however, grow elsewhere in the body including the conjunctiva. Conjunctival lymphomas are mostly of non-Hodgkin’s B-cell type. Follicular lymphoma is the next most common lymphoma. The lymphoma may just affect the conjunctiva or can affect other areas in the body as well.
b) What are the symptoms of conjunctival lymphoma?
Conjunctival lymphoma looks like a large “salmon pink” growth on the conjunctiva. This may cause grittiness, watering, or irritation to the eye.
c) Will I need any tests?
A biopsy is usually required to confirm the diagnosis. If we suspect the lymphoma is behind the eye or affecting else where in the body we may organise:
• Ultrasound scan
• CT scan
• MRI scan
d) What is the treatment for lymphoma?
After biopsy confirms the diagnosis of lymphoma, we may treat with:
• Radiotherapy
• Chemotherapy
Our choice of treatment is be guided by the haematologist or medical oncologist.
