What is a Tibial Fracture?
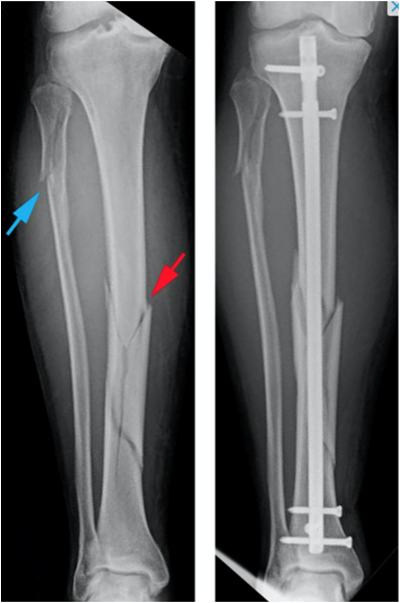
A fracture is a break or crack in a bone. The Tibia is the ”shin bone” in the lower leg, between the knee and ankle. The top of the tibia is the bottom half of the knee. The bottom of the tibia is the top half of the ankle. The fibula is a smaller bone that sits on the outside of the tibia. A tibial fracture is a break or crack in the tibia. It happens when a force is applied to the bone that is stronger than the bone can withstand.
This sometimes happens after a fall, playing sport, a road traffic accident or a fall from height. Occasionally the skin will be damaged at the same place as the fracture which is then called an ”open fracture”. Sometimes the fracture goes into the knee or ankle joint, which is then called an “intra-articular fracture”.
Why is my injury being treated with surgery?
The aim of surgery is to realign and stabilise the bone while it is healing. This is to try and prevent permanent stiffness, weakness and pain. Some tibial fractures can be treated in a plaster or splint if the bone is not displaced and stable, you accept the displacement or surgery would be too risky for you.
What does surgery involve?
Surgery usually involves the bone being realigned either through pulling the leg straight or with a clamp through small cuts in the skin. The bone is then held together with a metal rod that is put within the bone. This rod goes from just below the knee to just above the ankle. Screws lock the rod in place at the top and bottom. There are other ways that tibial fractures can be fixed surgically but your surgeon will discuss them with you if that is necessary. Usually the other methods are if you have an open or intra-articular fracture.
You will usually have a small cut (wound) at the front of the knee, two small stab wounds just below this and another 2 small stab wounds just above the ankle. If another wound is needed to realign the fracture with a clamp you may have another wound at the level of your fracture.
There are always risks of surgery, these will be explained to you before surgery takes place by your surgeon. Surgery will either involve a general anaesthetic (going to sleep) or a spinal anaesthetic (numbing your leg so you don’t feel the surgery). This will be decided between you and your anaesthetist. The surgery usually takes between 1-2 hours.
What Happens Next?
You will usually be discharged from hospital within a day or two after surgery unless you have problems with your mobility. Before you go home a doctor or nurse will discuss with you whether you need to take any blood thinning medication. You will usually have follow up at 2 weeks and 12 weeks after surgery. These appointments will should be given to you before you leave hospital.
Walking Boot : You will usually go home wearing a walking boot that you can put as much weight through as you are able. You should wear this for 2 weeks after surgery (you can wear this for up to 6 weeks if you find it helpful). You can take it off when you are sitting down, in bed, or doing your exercises.
Physiotherapy : You will also see a physiotherapist before you go home that will show you how to do some knee and ankle exercises. These are also shown in this information sheet. If they think you might need some extra help they will arrange an appointment for you to see them once you have gone home.
Follow Up Appointments
At around 2 weeks after your surgery, you will be seen by one of the fracture clinic nurses. They will examine your wounds and leg. They will look at your wound, remove the clips. They will then make sure you have another appointment booked for week 12 with the fracture clinic. If they are concerned they may ask you to come back later that day or the next day to see a surgeon.
At around 12 weeks after your surgery, you will come back to hospital for an X-ray and to see a surgeon. Most people will be discharged after this appointment to patient initiated return but some may need more appointments or a physiotherapy referral.
If your bone has not healed back together yet, some bloods will be taken at this clinic and you might be referred onto a specialist. They will then phone you at around 6 months after surgery to find out how you are doing and to review your tests. If your bone hasn’t healed you might be offered further surgery at around 1 year following your original operation. This is only required for around 1 in 20 patients.
What Problems Should I Look Out For?
Some problems patients can develop after surgery are infection, blood clots in the leg, poor bone healing, arthritis, knee pain, nerve damage, irritating or prominent metalwork, , knee or ankle stiffness, walking difficulties or poor balance. If you are suffering from any of the list below, it may mean you have one of these problems from your surgery.
- Infection – You might feel unwell or feverish with increased pain, swelling or stiffness in the knee or ankle. Sometimes the wound can become red, painful or start to leak. If you develop any of these problems contact the clinic using the contact details below. If it is out-with clinic hours and you feel unwell then go to your local Emergency Department.
- Pain – This can be caused by many problems. If your pain is getting worse or you still have moderate or severe pain more than 12 weeks after surgery and it hasn’t been discussed with your surgeon, then contact the clinic using the details below.
- Stiffness – If you are having problems with knee or ankle stiffness that is affecting your ability to do things at 12 weeks after surgery you should arrange physiotherapy using the details below.
- Swelling – If you have new or worse swelling after you have been to your final clinic appointment then contact the clinic using the details below.
- Breathing problems – For around 1 in 100 patients, a blood clot can form in the veins of the leg after surgery. This might cause pain and swelling in the leg. Very rarely a clot can travel to the lung through the bloodstream. This can give people chest pain or breathing difficulties. If you think you have one of these problems phone an ambulance or NHS24 immediately.
Walking difficulties or balance problems – There are different reasons why patients can have problems with walking or balance after surgery. If these problems continue for more than 12 weeks after surgery you may benefit from speaking to a healthcare professional. You may also have stiffness or pain that affects your ability to walk. If your problem is mainly caused by pain, you should contact the clinic. If it is mainly caused by stiffness, or you have balance problems, you should arrange to see a physiotherapist. It is ok to call the clinic to discuss this first if you are not sure.
Irritating or prominent metalwork – If you can feel a prominent lump around one of your scars, it might be that one of the screws has become loose. If this happens you should contact the fracture clinic.
If you have a problem related to your fracture or surgery that is not listed here but you would like to see someone about it then please contact the clinic using the details below.
Queen Elizabeth University Hospital Fracture Clinic
- Call: 0141 452 3210 (Monday – Friday, 9.00am – 4.00pm)
Victoria ACH Fracture Clinic
- Call: 0141 347 8754 (Monday – Friday, 9.00am – 4.00pm)
When Can I Walk Again?
This depends on your injury and the surgery you have. Your surgeon will advise you about this after your surgery. Most patients will be allowed to walk as their pain allows them immediately after surgery.
You will need to wear a walking boot while you are walking for the first 2 weeks after surgery but you can wear it for up to 6 weeks if this is helpful. You can take it off when you are sitting down, sleeping or doing your exercises. Sometimes people need to use crutches for some of this period. This will be assessed by a physiotherapist before you go home and sometimes at their clinics.
When Can I Return To Work?
This depends on the demands of your job. It is likely that you will require 2-3 weeks off to recover from the surgery and allow the discomfort to settle. If you have an office job, returning to work after this for light duties might be possible, but you should avoid anything which makes your ankle uncomfortable, such as prolonged standing or walking.
For manual work requiring lifting, you will need at between 6-12 weeks off, and this may be longer depending of the extent of your injury. If your job involves driving you will be off work for at least 6 weeks. Once you can do the activities required by your job without significant pain, you can go back to work.
When Can I Return to Driving?
You should not drive while you are in a cast or walking boot. You cannot drive for at least 6 weeks after surgery. After this you can drive when you are able to control your vehicle and safely perform an emergency stop. This is your decision. You can discuss this with your doctor or physiotherapist if you are unsure.
You must be safe and in control of the vehicle. The law is very clear that you have to be able to prove to the police that you are ‘safe’ to drive, so it is entirely your own responsibility and we cannot give you permission to drive.
When Can I Return To Sport?
You should only return to contact sport at least 12 weeks after your injury. Other sport may be possible earlier but you should take the advice of your doctor or physiotherapist who will guide you.
Do I Need Physiotherapy?
Before you are discharged you will be seen by a physiotherapist and they will go over the exercises in this book with you. If they feel that you might need extra help they may arrange an appointment at their clinic for you.
If you are having problems with stiffness and this is affecting what you can do discuss this at your clinic appointment and you may need a physiotherapy referral. If you have been discharged from Orthopaedic clinic, please contact the physiotherapy department below or arrange this with your GP.
What Will My Recovery Be Like?
Below is a rough guide of what most patients will be able to do after surgery for a tibial fracture. Everyone is different and some people may take longer or shorter to be able to do these things. If you are unsure please discuss them with your nurse or surgeon.
Weeks 0 to 2
- You will be in a walking boot for 2 weeks (up to 6 weeks if you find if helpful).
- Keep foot elevated when you are not walking to reduce swelling.
- You can weight bear as your pain allows.
- You can remove this when you are sitting down, in bed or doing your exercises.
- You can begin the knee and ankle exercises.
Weeks 2 to 6
- Continue knee and ankle exercises
- Return to desk based work if required and comfortable.
Weeks 6 to 12
- The fracture is still healing.
- You can begin to resume normal activity but be guided by any pain you are experiencing.
- Carry out day to day activities.
- Continue knee and ankle exercises.
- If you no longer require to wear a walking boot you may wish to consider driving provided you can safely operate a car.
- Heavy tasks, heavy lifting or sport may cause some initial discomfort.
Week 12+
- The fracture is still healing for most people. It is usually healed by around week 14.
- Return to manual work, sport and heavy activities may be possible.
- If you are still experiencing significant pain or swelling that has come on after your week 12 clinic appointment then please contact the fracture clinic for advice.
Exercises
Daily exercise programme
Aim to complete this exercise program every day, five times daily. You should spend around 2 minutes per exercise.
Bed Exercise
1. Straight leg raise

- Sit in bed with your legs straight and your back supported
- Point your toes up to the ceiling, tighten your thigh muscles of your operated leg and press the back of your knee down into the bed.
- Keep the knee straight and lift your leg up off the bed (clearing approx 30cm)
- Hold for five seconds and then relax for five seconds.
- Repeat 10 times
2. Ankle Movement

- Sit in bed with your legs straight and your back supported.
- Write out the alphabet with your foot, allowing your ankle to move through the movements of all the letters A to Z. All the movements should come from your ankle joint
3. Active assisted toe up with towel

- Sit in bed with your legs straight and your back supported.
- Loop a long towel/cloth around the front of your foot.
- Hold the two ends with your hands.
- Keeping you knee straight, try to bring your toes up towards your face. Assist the movement by pulling the ends of the towel/cloth.
- Hold this position for 30 seconds and then release and relax.
- Repeat 10 times
Chair Exercises
1.Knee bending

- Sit upright in a chair, with both feet flat on the floor.
- With the operated leg, slide your foot underneath the chair, keeping your toes on the floor, trying to bend your knee as much as possible, within your pain limits.
- Hold this bent position for 10 seconds and then slowly return your leg to a comfortable position.
- Relax between repetitions.
- Complete this exercise 10 times.
2. Knee extension

- Sit in a chair, with your knees at 90 degrees, and with both feet on the floor.
- With the operated leg, tighten the muscles in your thigh, lift your toes and straighten your leg as much as possible.
- Hold this straight position for five seconds and then slowly lower back down to the floor.
- Relax between repetitions.
- Repeat 10 times.
Patient Initiated Return
At the end of your final appointment you will usually be discharged from further follow up. This information sheet has advice on problems to watch out for and advice on exercises you should carry out. You should read through this leaflet closely as they will tell you about what you should expect for your recovery. They will also tell you how to get arrange a further appointment should you have any problems.
Once you have finished at your final appointment, if you develop a problem related to your tibial fracture or surgery, you can contact the clinic and arrange a new appointment yourself. You do not need to contact your GP to do this.
Further Information and Contact Details
Contact Details
- Queen Elizabeth University Hospital main switchboard – 0141 211 1100
- Queen Elizabeth University Hospital Fracture Clinic – 0141 452 3210 (Monday – Friday, 9.00am – 4.00pm)
- Victoria ACH Fracture Clinic – 0141 347 8754 (Monday – Friday, 9.00am – 4.00pm)
- Appointments booking office – 0141 347 8347 (Monday – Friday, 8.00am – 8.00pm)
- Physiotherapy – 0141 452 3713 (Monday – Friday 8.30am – 4.00pm)
- MSK Physiotherapy Self Referral
Other Resources
- Further information is available on the NHS UK website
